Quality, Access, and the Use of Real-World Data by Payers: Where Are We Now? Where Do We Want to Be in the Future?
Brian O’Rourke, PharmD, Chair of the ISPOR HTA Council, Ottawa, Ontario, Canada; H. Arturo Cabra, MSc, ISPOR, Lawrenceville, NJ, USA; Lucinda S. Orsini, DPM, MPH, ISPOR, Lawrenceville, NJ, USA (now with COMPASS Pathways, New York, NY, USA);
John Guerino, MHS, ISPOR, Lawrenceville, NJ, USA
One of the biggest challenges payers face today is determining the value of innovative therapies in diseases with high unmet medical needs, such as cancer and rare diseases. These novel therapies show promise, but there is often significant uncertainty regarding their added value to patients and their cost to the healthcare system. In some cases, the new therapies front-load most of the cost as is seen with gene and cell therapies. This creates strain on healthcare system budgets, raises affordability and equity issues, and challenges decision making by health technology assessment (HTA) bodies and payers. Some payers are addressing this challenge by providing conditional reimbursement and employing risk-sharing strategies via managed entry agreements (MEAs). Although most MEAs promise predictable budget impact, there is also a move towards the development and application of performance- or outcomes-based MEAs. To support the implementation of outcomes-based agreements, HTA bodies and payers are increasingly looking to collect and analyze real-world data (RWD).
Barriers to Overcome
The ISPOR Payer Summit was developed in collaboration with a group of dedicated volunteers representing a cross-section of stakeholders. The Summit was an invitational, multistakeholder event to discuss the use of real-world evidence (RWE) by public and private payers in the United States and Canada. The Summit was moderated by Clifford Goodman, PhD, Senior Vice President, Comparative Effectiveness Research, The Lewin Group, Falls Church, VA, USA. It began with expert summaries of 2 prerecorded presentations from Sebastian Schneeweiss, MD, ScD, Harvard Medical School, Boston, MA, USA, and Francesca Cunningham, PharmD, Director of the Center for Medication and Safety at the US Department of Veterans Affairs, Hines, IL, USA.
"Ideally, the future of using real-world evidence for coverage decisions requires clearly defined terminology and processes to broadly integrate data (including patient-generated data)."
Dr Schneeweiss highlighted some of the barriers that payers face in using RWE. He noted, “Payers make high-impact healthcare decisions all the time, yet they underutilize their very own data to identify what works in their population. They often have little confidence in RWE and lack capacity to produce it at scale in real time with their own data.” However, he suggested the use of modern rapid-cycle analytic platforms can help overcome these barriers. Schneeweiss proposed the use of a Meaningful, Valid, Expedited, and Transparent evidence framework (MVET framework)1 to instill confidence in using RWD for decision making. He presented several examples, including a study that showed improved health outcomes and total cost of care when using SGLT-2s in high-risk cardiovascular disease patients with diabetes based on data from the very population that the health plan manages rather than an external finding.2 “While there are some considerations involved in using RWE to support reimbursement decisions, the benefits are significant. Without the use of RWE, payers are left with making substantial extrapolations from randomized controlled trial evidence,” Schneeweiss said.
Using Data for Better Patient Outcomes
Dr Cunningham discussed several ways that the US Department of Veterans Affairs (VA) uses its data to better understand safety and effectiveness outcomes for its patients. She highlighted some of the decisions made in real time using VA databases, data warehouses, and electronic health records (EHRs), together with an assortment of dashboards. She explained that the VA uses RWD in many ways: (1) to conduct active and passive safety surveillance; (2) to support national medication use evaluations (MUEs); (3) to populate risk reduction dashboards; (4) to inform formulary management, including responses to complex queries and traditional formulary decisions; and (5) to develop research proposals.
Cunningham presented one example that focused on COVID-19 and the ability of the VA to evaluate and characterize utilization of diagnostic testing and various treatments for the virus. This allowed them to provide pertinent and timely information, including detailed safety monitoring of medications to decision makers and healthcare providers. She also provided background on their evaluation of several potential therapies proposed to treat patients during the pandemic. Using a lesson learned approach, the VA identified several areas to improve the use of RWD such as: (a) the need to enhance database connectivity and interoperability; (b) a requirement to develop new methods and tools to address different types of questions; (c) and a need to efficiently capture data and develop the tools necessary to answer the question at hand. She stressed the importance of understanding the limitations of administrative data and highlighted the benefits of developing tools to enhance the use of data.
The participants were then divided into 4 discussion groups. Two groups focused on the current landscape of using RWD in coverage decisions, and 2 groups focused on the future landscape. Participants were asked to answer the following questions:
• Current landscape
“What is the current landscape of using RWD in coverage decisions? What is preventing impactful use of RWD/RWE in the current environment by payers?”
• Future landscape
“What does the ‘ideal’ future of using RWD/RWE in coverage decisions look like? Where do we want to be? How do we get there (the future ideal)? What big changes, collaborations, or data linkages would have to take place?”
Results From the Current Landscape Breakout Groups
While most agreed that more could and should be done with RWE in payer decision making, most of the barriers discussed that are preventing further application of RWE are not new—they involve many of the same challenges discussed for many years. Where there is use of RWD, it is still unclear how it is informing decisions in real time. Current usage of RWE includes developing prior authorization criteria and supporting appeals (including how the process has changed over time), new data collection to supplement HTA or to reassess technologies, exploratory or population-level health management including disease state information (often for orphan diseases), conditional reimbursement and value-based agreements, and reporting of patient experience particularly for specialty pharmacy products.
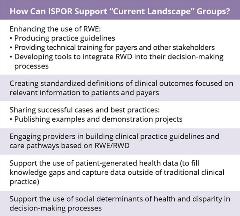
The groups felt that ISPOR can support enhanced use of RWE by producing practice guides, providing technical training for payers and other stakeholders, and by developing tools to integrate RWD into decision-making processes. Other opportunities highlighted included creating standardized definitions of clinical outcomes focused on relevant outcomes to patients and payers; publishing examples and demonstration projects; and engaging providers in building or amending clinical practice guidelines and care pathways based on RWD/RWE. There was also discussion about using data captured outside traditional clinical practice, such as patient-generated health data, to fill knowledge gaps, as it was thought that patient-generated data are still very underutilized. And finally, the use of social determinants of health and disparity data were also identified as being important factors in decision making.
Results From the Future Landscape Breakout Groups
Ideally, the future of using RWE for coverage decisions requires clearly defined terminology and processes to broadly integrate data (including patient-generated data). RWD should be used by regulators and HTA bodies to conduct rolling reviews and to “evergreen” technology assessments. These reassessments can then be used to modify reimbursement criteria, renegotiate prices, and eventually to support disinvestment decisions.

To gain the confidence of payers and other stakeholders, these data must be of high quality, replicable, robust, and transparent and should include the most relevant variables and adequate sample sizes. Participants felt that RWD should ideally be used to translate clinical trial efficacy into relevant real-world effectiveness and cost-effectiveness on a routine basis, as well as to monitor real-world effectiveness over time. There should be an ongoing data stream with real-time “dashboard” analytic capabilities to query and report data as needed by payers and providers, perhaps using predefined algorithms and artificial intelligence platforms. There should be processes to enhance communication amongst stakeholders about product or service performance. This will also require an underlying knowledge and acceptance of the quality and relevance of RWE by end users and how best to put it into context of the data continuum. A collaborative approach to research and an ability to leverage capabilities from different stakeholders is also required.
You Can Get There From Here
So, how do we get there? Data linkages and universal patient identifiers will enhance the ability to create the robust all-inclusive datasets envisioned by this ideal future. In addition, a networked data pool (pond, lake, ocean), similar to the US Food and Drug Administration’s (FDA’s) Sentinel initiative, based on an open data platform that is available to all key stakeholders will be beneficial. This will require a realignment of incentives and priorities as well as resources to develop and maintain the platforms, manage the input of data, download and analyze the data, and build real-time analytics and end-user capabilities to interpret the resulting output.
How Can ISPOR Help?
ISPOR brings together many different perspectives and stakeholders in industry, regulators, HTA agencies, payers, providers, academics, and patient groups that will be instrumental to solving some of the challenges raised in this summit. Certainly examples, guidance, and tools for implementing RWE in decision making are ways that ISPOR has and will continue to make a difference in this space. But education and training of relevant and competent RWE data scientists, epidemiologists and outcomes researchers cannot be underestimated. Developing a competency framework for these experts in training will be essential, while also continuing to provide training opportunities through short courses, webinars, and event workshops.
Some specific points ISPOR can address going forward include:
1. Promote collaboration among stakeholders (industry, regulators, HTA agencies, payers, providers, academics, and patient groups)
One of the powers that a professional association like ISPOR possesses is the ability to promote interaction and collaboration among stakeholders. The safe havens provided by meeting together outside of the promotional space allows for constructive dialogue on topics that impact all participants, including ideas and recommendations on how to work collaboratively to move beyond the barriers identified.
2. Provide education and training
ISPOR, as a global scientific and educational organization for health economics and outcomes research, is well positioned to offer training related to RWE. Understanding that the capacity to analyze and interpret data in this context is at a premium, ISPOR can create opportunities for payers, clinicians, researchers, and patients to enhance their knowledge in the application of RWE.
3. Disseminate RWE case studies, guidance documents, and tools to promote broad adoption
ISPOR should gather actual examples of RWE use in coverage decisions. These examples can help identify opportunities and challenges to the use of RWE in decision making. ISPOR can also work with experts and stakeholders to develop guidance documents and tools to harmonize approaches to the collection and use of RWE and to contextualize RWE use based on local needs. This will require a concerted effort by all stakeholders to bring together the various “data owners” (companies, private and government insurers, academic data aggregators, and patient organizations). ISPOR can help support the creation of these linkages.
4. Champion RWE initiatives that incorporate patient perspectives
ISPOR works with individual patient representatives and patient groups to ensure that the patient voice remains a key input to market access, and that should include how RWE is employed in coverage decisions. Patients are generating healthcare data through their interactions with providers and insurers. However, the increased use of data from wearables, healthcare apps, and other social media-derived datasets is becoming increasingly integral to this discussion. Patients and patient groups need to be directly involved in the effort to increase the acceptance of patient-generated data. ISPOR remains committed to elevating patient involvement in these initiatives.
References
1. Schneeweiss S, Eichler HG, Garcia-Altes A, et al. Real world data in adaptive biomedical innovation: a framework for generating evidence fit for decision-making. Clin Pharmacol Ther. Dec;100(6):633-646. doi: 10.1002/cpt.512. PMID: 27627027.
2. Garry EM, Schneeweiss S, Eapen S, et al. Actionable real-world evidence to improve health outcomes and reduce medical spending among risk-stratified patients with diabetes. J Manag Care Spec Pharm. 2019; 25(12):1442-1452. doi: 10.18553/jmcp.2019.25.12.1442. PMID: 31778623.
Explore Related HEOR by Topic

