Improving Access to Care and Support for Mental Health Conditions: A Call to Action
Lucinda S. Orsini, DPM, MPH, Vice President, Value and Outcomes Research, COMPASS Pathways, Skillman, NJ, USA
The occurrence of mental health disorders is growing at an increasing rate with pervasive consequences at both the personal and population levels. Brain health is a key component of our overall health. As Director-General of the World Health Organization (WHO) Tedros Adhanom Ghebreyesus, MSc, PhD said, “Ultimately, there is no health without mental health.” The WHO defines brain health as “a state in which every individual can learn, realize their potential, and optimize their cognitive, psychological, neurophysiological, and behavioral responses, while adapting to changing environments”.1 The WHO has included mental health in its sustainable development goals, recognizing that global [health and economic] development targets cannot be achieved without attending to mental health issues introducing global objectives as part of a comprehensive mental health action plan.2 There is also an ongoing special initiative (2019–2023) for mental health, calling for universal coverage for mental health services with the goal of ensuring access to quality and affordable care for mental health conditions in 12 priority countries.3
These advocacy efforts were already in play prior to the COVID-19 outbreak. The pandemic has only intensified the mental healthcare crisis and increased the urgency to recognize and address the widening gaps between our behavioral and mental healthcare needs and the available coverage and treatment. To provide services, we need to understand the magnitude of the problem and appropriate the correct resources toward rectification. However, the data that we have regarding the size and demographics of mental health disorders need to be interpreted with caution. While long-standing global studies offer the best available evidence, they remain uncertain due to a lack of evidence in many countries. Estimates are often based on incomplete input data that do not cover all parameters or all countries, as well as information that is outdated or poor quality. According to the WHO’s report on mental health, “it is important to acknowledge that mental disorders can be conceptualized in different ways across cultures, which raises challenges for measuring them from a particular reference point, such as in the global burden of disease studies.”4
"The pandemic has only intensified the mental healthcare crisis and increased the urgency to recognize and address the widening gaps between our behavioral and mental healthcare needs and the available coverage and treatment."
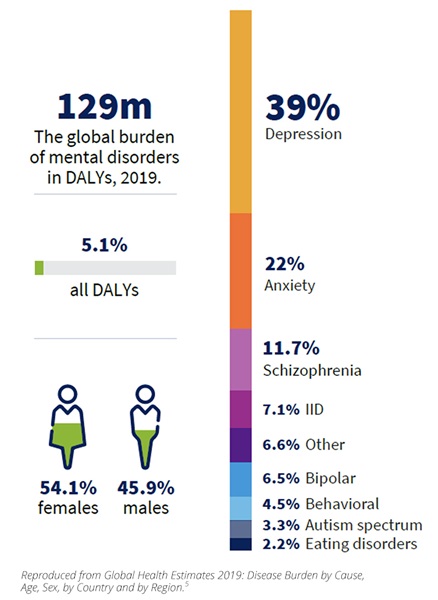
Figure 1, replicated from the World Mental Health Report: Transforming Mental Health for All,4 shows that 970 million people are living with mental health disorders worldwide and anxiety and depressive disorders are the most common issues from which people suffer. Rates of depression rise worldwide as the population ages—among adults, depression is the most prevalent of all mental disorders.4 The COVID-19 pandemic has also had an impact with estimates of increases of 28% in the prevalence of depression and 26% increase in the prevalence of anxiety between 2019 and 2020.4 Mental health disorders are a leading cause of disability worldwide with depression being the major contributor to the burden of disability-adjusted life years (DALYs) (Figure 2).5 Depressive disorders alone are the second-leading cause of years lived with a disability among all causes of disabilities globally, followed by back and neck pain.5 Major depressive disorder (MDD) is also the leading cause of disability in the United States.6
Figure 1. The global prevalence of mental disorders in 2019

Figure 2. The global burden of mental disorders in disability-adjusted life years (DALYs), 2019
MDD is challenging to treat due to the episodic nature of occurrence and the varied set of symptoms that people experience. A combination of factors—including genetic, biological, environmental, and psychological factors—contributes to the risk for developing depression. MDD is often a chronic disease in which the episodes vary in severity and duration. Symptoms can be severe enough that they impact daily life and individual function; in its most severe form, depression can become life-threatening.7,8 In some cases, people with MDD do not respond adequately to treatment, leaving them with persistent symptoms and higher risk of relapse.9 MDD that isn’t helped after 2 or more adequate antidepressive treatments of adequate dose and duration is referred to as treatment-resistant depression (TRD). There is a 20% to 30% prevalence of TRD among people with MDD.10,11 People with TRD are more likely to exhibit suicidal ideation, intent, and attempts.
Worldwide 1 person dies from suicide every 40 seconds with 20 attempts for every death.12 While globally the suicide rate has decreased since 2000, the suicide rates in the Americas have increased 17% over the past 20 years, ranking as a top 10 leading cause of death in the United States and is the leading cause of death in young adults.4 Risk of suicide increases with severe and persistent mental disorders.13 Approximately 90% of individuals who die from suicide in the United States have an underlying mental illness, and about half of those suffer from MDD.14,15 People exhibiting suicidal ideation, intent, and attempts account for a majority of emergency room and hospital admissions for reasons related to mental health.
In terms of economic consequences, a systematic review of cost of illness studies from many countries showed that the average annual cost of mental health conditions per person ranged between $1180 and $18,313 depending on which condition they experienced.16 This number accounts for direct and indirect costs. Annual spending on mental healthcare in the United States accounts for approximately 5% of total healthcare spending, with governmental payers (eg, Medicare and Medicaid) picking up ~75% of the costs.17 While schizophrenia tends to be the costliest mental health condition, depressive and anxiety disorders which are often comorbid, are much more prevalent and account for the majority of overall national mental health spend.16 People with TRD tend to incur higher levels of healthcare utilization compared to people with non-TRD MDD, including higher nonmental health-related healthcare costs which actually form the larger proportion of overall spending.18 Inpatient and outpatient costs are the highest drivers of healthcare spend for both TRD and MDD.
"We need to prioritize mental health and serious mental illness in our research programs. This is a call to action to put a spotlight on this highly prevalent and growing issue."
In summary, mental health conditions are ubiquitous, costly, and often severely underserved. The WHO has highlighted 4 main gaps in our ability to address this crisis in its world mental health report.4 The first is the information gap that consists of incomplete or lacking data on the scope of the issue as well as insufficient research into these issues. The second is a governance gap that includes inadequate policies, plans, and laws, along with misplaced priorities on interventional care versus prevention. The third is a resources gap consisting of scant spending, lack of essential medicines, scarce workforce, and the digital divide which means telehealth and digital solutions remain out of reach of many. The fourth gap is in access to services—both poor treatment coverage and limited range and quality of services.
Health economics and outcomes researchers have an opportunity to help inform or fill many of the gaps that are mentioned here. Focus on the information/data gaps are what we do best in terms of applying evidence to scoping the issue both in terms of size and costs. This evidence can then be applied to inform the governance gap to show how reprioritizing resources could impact outcomes and the overall healthcare spend. Changes in governance can influence incentives for coverage of medications/services and perhaps incentivize innovation in this space which is sorely needed. Incentives can also influence workforce development and infrastructure to ensure more people have access to the care they need. This can begin to shift access to services and eventually improve the quality of services offered. However, we need to prioritize mental health and serious mental illness in our research programs. Most everyone either has lived experience, knows, or is caring for someone with a mental health condition at this moment. This is a call to action to put a spotlight on this highly prevalent and growing issue. We need to come together to work on these challenges to improve access to care and support for mental health conditions. We ignore these issues at our own peril.
References
1. World Health Organization. Intersectoral Global Action Plan on Epilepsy and Other Neurological Disorders 2022-2031. Accessed April 20, 2023. https://www.who.int/publications/m/item/intersectoral-global-action-plan-on-eepilepsy-and-other-neurological-disorders-2022-2031
2. World Health Organization. Mental Health. Accessed April 20, 2023. https://www.who.int/health-topics/mental-health#tab=tab_1
3. World Health Organization. The WHO Special Initiative for Mental Health (2019-2023): Universal Health Coverage for Mental Health. Accessed April 20, 2023. https://apps.who.int/iris/handle/10665/310981
4. World Mental Health Report: Transforming Mental Health for All. Geneva: World Health Organization; 2022. License: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications/i/item/9789240049338
5. Global Health Estimates 2019: Disease Burden by Cause, Age, Sex, by Country and by Region., 2000–2019. Geneva, World Health Organization; 2020. Accessed April 25, 2023. https://www.who.int/docs/default-source/gho-documents/global-health-estimates/ghe2019_yld_global_2000_2019c417f68b-841d-4a7a-9e5c-f087f9f86e48.xlsx?sfvrsn=dac29788_7
6. Kessler RC. The costs of depression. Psychiatr Clin North Am. 2012;35(1):1-14.
7. Healthline. Signs and Symptoms of Mild, Moderate, and Severe Depression. Accessed June 16, 2021. https://www.healthline.com/health/depression/mild-depression
8. Healthline. How Long Does Depression Last? Accessed June 16, 2021. https://www.healthline.com/health/how-long-does-depression-last
9. Johnston KM, Powell LC, Anderson IM, Szabo S, Cline S. The burden of treatment-resistant depression: A systematic review of the economic and quality of life literature. J Affect Disord. 2019;242:195-210. doi: 10.1016/j.jad.2018.06.045
10. Fostick L, Silberman A, Beckman M, Spivak B, Amital D. The economic impact of depression: Resistance or severity? Eur Neuropsychopharmacol. 2010;20(10):671-675. doi: 10.1016/j.euroneuro.2010.06.001
11. Lin J, Szukis H, Sheehan JJ, et al. Economic burden of treatment-resistant depression among patients hospitalized for major depressive disorder in the United States. Psychiatr Res Clin Pract. 2019;1(2):68-76. doi: 10.1176/appi.prcp.20190001
12. Suicide Worldwide in 2019: Global Health Estimates. Geneva: World Health Organization; 2021. License: CC BY-NC-SA 3.0 IGO.
13. CDC. Suicide rising across the US. Published 2018. Accessed June 16, 2021. https://www.cdc.gov/vitalsigns/suicide/
14. NAMI. Mental Health Facts. Accessed June 16, 2021. https://www.nami.org/mhstats
15. American Foundation for Suicide Prevention. Suicide claims more lives than war, murder, and natural disasters combined. Accessed June 16, 2021. https://afsp.donordrive.com/index.cfm?fuseaction=cms.page&id=1226&eventGroupID=9
16. Christensen MK, Lim CCW, Saha S, et al. The cost of mental disorders: a systematic review. Epidemiol Psychiatr Sci. 2020;29:e161. doi:10.1017/S204579602000075X
17. Mental Health America. Paying for Care. Accessed June 16, 2021. https://www.mhanational.org/paying-care
18. Amos TB, Tandon N, Lefebvre P, et al. Direct and indirect cost burden and change of employment status in treatment-resistant depression. J Clin Psychiatry. 2018;79(2):17m11725. doi: 10.4088/JCP.17m11725.