Institutional Country-Specific Context and Value Drivers in Health Technology Assessment
- A European Perspective
Jeffrey M. Muir, MSc, DC, MSc; Amruta Radhakrishnan, MPH; Cytel, Inc, Toronto, Ontario, Canada; Andreas Freitag, MD, MSc, Cytel, Inc, London, England, UK; Ipek Ozer Stillman, MBA, Takeda Pharmaceuticals, Lexington, MA, USA; Grammati Sarri, PhD, Cytel, Inc, London, England, UK
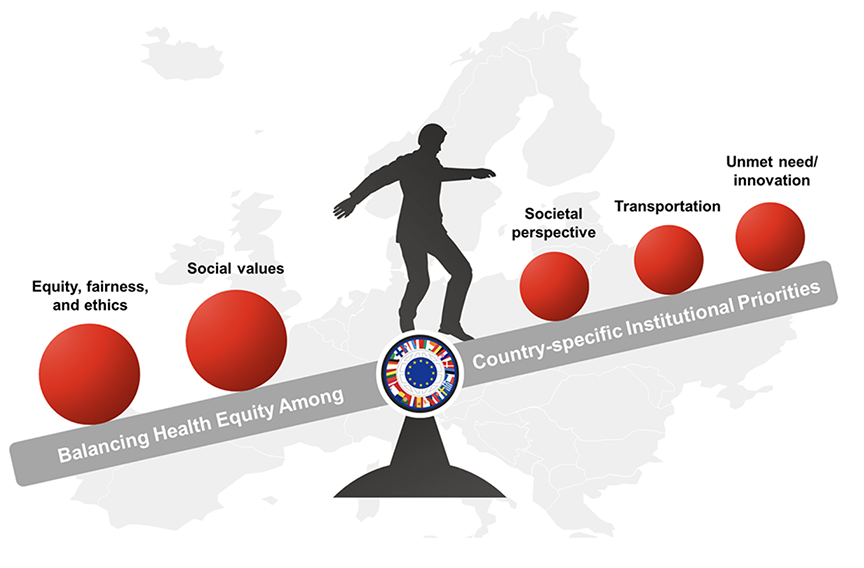
Health technology assessments (HTAs) are a cornerstone of healthcare decision making across many countries, each of which applies various context-specific criteria in their evaluations. Traditionally, clinical- and cost-effectiveness are the main drivers of determining the added value of a new treatment. Recently, though, there has been an effort to expand the elements considered during HTA, with an added focus on what are considered “additional” elements of value.1 This can be considered an extension of the “go beyond health” concept championed by Engel et al,2 who first suggested that HTA agencies consider factors beyond the mere improvement of health outcomes when evaluating new therapies (Figure 1).
Figure. Elements addressing health equity must be balanced against the demands of country-specific institutional priorities.
The challenge in incorporating these additional elements in multijurisdictional HTA efforts, however, is to achieve a fully harmonized approach in a climate where criteria outlining what constitutes “value” and the methods to assess these value elements differ from country to country.
This challenge is especially prescient in the European Union (EU), where the 27 member states each apply their own criteria and evaluation processes, involving varying regulatory bodies and jurisdictional differences3 and complicated by the differing approaches to healthcare system design throughout the European Union.4 Indeed, much effort has been spent examining access to healthcare and the inequities that exist across the different EU member states,5 towards a goal of providing equal access to all citizens, regardless of socioeconomic standing.6 In an effort to standardize the pan-EU assessment process, the Joint Clinical Assessment (JCA) has been proposed.7 This effort seeks to provide a common approach to HTA, one designed to create efficiencies and accelerate the availability of new treatments across European citizens. The proposed JCA will provide a uniform set of factors to assess the clinical value of new technologies while leaving interpretation of the findings to be jurisdiction-specific, such that each HTA body would remain responsible for determining the potential added value of a therapy based on their specific healthcare system.7
Full implementation of the JCA guidelines is slated for early 2025; however, in the lead-up to this, it is important to evaluate the current decision-making climate and, in the context of additional aspects of technology value, to determine what elements are currently considered as part of the various HTA agencies. The published literature reveals wide variations between EU member states on the decision criteria and suggests, among other determining factors, that 2 main considerations will govern the ease with which the JCA guidelines will be accepted: (1) the willingness of a member state to include elements of value beyond clinical effectiveness, and (2) the institutional context for each member state.8
"There has been an effort to expand the elements considered during HTA, with an added focus on what are considered “additional” elements of value."
Willingness to Include Elements of Value
Value elements beyond the purely clinical or economic are numerous and varied. Novel value elements include factors that can be quantified directly (such as environmental impact, productivity, transportation, etc) as well as factors that are perceived as less quantifiable (such as the value of hope, real option value etc.). Several of these novel elements are widely reported in the literature and thus represent core values considered by many countries, while others are more rarely included and could be considered emerging philosophical topics. Among EU member states, equity or fairness sits atop the list. Elements that consider the social value of a new therapy or whether the social perspective is addressed by a new therapy were also frequently considered. These 3 elements could be grouped loosely under the umbrella of “societal considerations,” as they examine the impact of a potential new therapy on society itself and are widely recognized. The societal net could be cast farther to include several other elements that are relatively commonly incorporated: whether the therapy will impact society’s (and patients’) productivity, whether indirect factors are taken into consideration, and whether the therapy will impact transportation within a society (ie, the ability of that society to continue to be mobile).
In the European landscape, these elements—all of which address the impact of a new therapy on the societal fabric—are often considered, suggesting that their value is real and recognized. There are a number of elements that are, in contrast, considered by very few countries. Elements such as environmental impact, adherence-improving factors, and disease severity are considered intermittently, indicating that their value cannot be clearly established in a broader multijurisdictional framework and thus would require reconsideration or further research to determine their real value. Finally, there are elements of value that may be considered “emerging elements” that are considered very rarely.1,9 Interestingly, these elements tend to reflect a societal perspective and the value of a given therapy for the patient and their overall well-being, beyond that which is provided by the therapy. As such, their rare inclusion is curious, as they fall under the umbrella of elements that have historically been viewed as important. Real option value, or the potential benefit from other interventions realized by extending the patient’s life, is rarely considered. While other elements such as the value of hope and the reduction of uncertainty—valuable elements that may not realize a tangible return on investment but nevertheless provide patients with hope and thus may provide an additive factor to a new therapy—are almost never mentioned. This also holds true for the impact of a given therapy on the capacity of the healthcare system. That these elements are considered in such low numbers, especially given their societal impact and the obvious value of societal perspective to most EU member states, represents a missed opportunity in HTA decision making.
Elements of Value and Institutional Context
Constitutional context exerts substantial influence over the incorporation of elements of value into HTA decision making. There is evidence that the maturity of the healthcare system in part governs the ability to incorporate additional elements of value, with less mature HTA organizations often “lacking the expertise and resources to assess societal and novel elements.”10
Of the 25 EU member states where research data are available, 9 have a Beveridge-type national healthcare system, 8 have a social health insurance system based on the Bismark model, and the remaining 8 have a system that would be considered “in transition.”4 Perhaps not unexpectedly, countries with a robust national health system tend to incorporate more elements of value, whereas countries with systems in transition consider fewer elements. Countries using a social health insurance system offer a more robust offering than those in transition but do not match the commitment of national healthcare system-style countries.
Regardless of institutional context, there is some consensus among EU member states on the most important additional value elements, namely equity/fairness and social values. Likewise, societal perspectives and unmet needs are considered in the vast majority of countries, regardless of healthcare system. Where things diverge is in the incorporation of the “second tier” of societal elements, such as productivity considerations, transportation impact, etc. Countries with more mature, robust healthcare systems tend to incorporate these elements, while those in transition do so much less frequently. This trend is even more noticeable in the context of emerging elements that tend to be considered in only the most robust and comprehensive countries.
"There is substantial variation in how different EU member states apply elements of value in HTA, which only adds to the challenges associated with applying a uniform set of standards to a diverse and varied group of jurisdictions."
Clearly, there is substantial variation in how different EU member states apply elements of value in HTA, which only adds to the challenges associated with applying a uniform set of standards to a diverse and varied group of jurisdictions. The incorporation of additional value elements into HTA decision making will also require sufficient and suitable data which are unlikely to be available across all jurisdictions. The willingness of a member state to adopt elements beyond the merely clinical and/or economic in HTA deliberations is at least partially tied to the healthcare construct employed by that country. We have seen that countries with more mature and robust health systems are more willing to broaden the criteria used in their discussions, perhaps with the understanding that, as the main funder of the system, their willingness to consider a broad range of factors may ultimately result in better outcomes and therefore improve the return on their investment. Conversely, countries with systems in transition have been seen to take a minimalist approach and look essentially at unmet needs alone. This is perhaps not unexpected for countries in transition, although it does underscore the challenge of applying the JCA guidelines on a broad scale.
Lessons Learned
There are challenges ahead in the implementation of the JCA guidelines for HTA agencies in the European Union. The current jurisdictional differences in institutional design and value drivers create disparities among the member states that create inequalities for their citizens. Understanding and addressing the variability of HTA acceptance drivers at a more granular level is key from the perspective of equal patient access to (innovative) treatments across Europe, to ensure that different trends in value considerations between national assessments do not threaten the weight of EU JCA in local HTAs and decision making. Chief among the challenges ahead is the variability of value considerations across national assessments within the European Union, with member states prioritizing various aspects of value. While the use of clinical and cost-effectiveness is widespread across the European Union, other elements, such as equity, fairness, social value, environmental impact, productivity, and the value of hope are only considered sparingly and in varying degrees. This diversity in value drivers can lead to discrepancies in the evaluation of new treatments and ultimately to patient access.
"Sharing best practices, lessons learned, and successful strategies for incorporating diverse value elements can promote a more unified and effective approach to HTA decision making."
To overcome these challenges, HTA agencies must aim for a more harmonized approach that considers a comprehensive range of value elements. Standardizing data collection methods and assessment frameworks can facilitate meaningful comparisons and ensure the credibility of HTA outcomes across member states. Efforts should also focus on enhancing transparency and collaboration among HTA agencies within the European Union. Sharing best practices, lessons learned, and successful strategies for incorporating diverse value elements can promote a more unified and effective approach to HTA decision making.
References
1. Muir JM, Radhakrishnan A, Freitag A, Ozer Stillman I, Sarri G. Reconstructing the value puzzle in health technology assessment: a pragmatic review to determine which modelling methods can account for additional value elements. Front Pharmacol. 2023;14:1197259. doi:http://doi.org/10.3389/fphar.2023.1197259
2. Engel L, Bryan S, Whitehurst DGT. Conceptualising “benefits beyond health” in the context of the quality-adjusted life-year: a critical interpretive synthesis. Pharmacoeconomics. 2021;39(12):1283-1395. doi:https://doi.org/10.1007/s40273-021-01074-x
3. Xoxi E, Di Bidino R, Leone S, Aiello A, Prada M. Value assessment of medicinal products by the Italian Medicines Agency (AIFA) and French National Authority for Health (HAS): similarities and discrepancies. Front Med Technol. 2022;4:917151. doi:https://doi.org/10.3389/fmedt.2022.917151
4. Jakubowski E, Busse R. Healthcare systems in the EU: A comparative study. 1998. Public Health and Consumer Protection Series. https://www.europarl.europa.eu/workingpapers/saco/pdf/101_en.pdf
5. Palm W, Webb E, Hernández-Quevedo C, et al. Gaps in coverage and access in the European Union. Health Policy. 2021;125(3):341-350. doi:https://doi/org/10.1016/j.healthpol.2020.12.011
6. Mazeikaite G, O’Donoghue C, Sologon DM. What drives cross-country health inequality in the EU? Unpacking the role of socio-economic factors. Soc Indic Res. 2021;155:117-155. doi:https://doi.org/10.1007/s11205-020-02587-2
7. Safety D-GfHaF. Implementing the EU Health Technology Assessment Regulation. Accessed February 5, 2024. https://health.ec.europa.eu/publications/factsheet-implementing-eu-health-technology-assessment-regulation_en
8. Radhakrishnan A, Muir JM, Freitag A, Mehra M, Ozer Stillman I, Sarri G. Exploring the link between institutional country-level differences and consideration of additional value elements in HTAs: results from a pragmatic review. Presented at ISPOR Europe 2023; November 12-15, 2023; Copenhagen, Denmark. Value Health. 2023;26(12 Suppl):S328. https://www.valueinhealthjournal.com/article/S1098-3015(23)04858-1/abstract?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS1098301523048581%3Fshowall%3Dtrue
9. Muir JM, Radhakrishnan A, Freitag A, Ozer Stillman I, Sarri G. Which modelling methods can account for additional value elements in HTAs? Results from a pragmatic review. Presented at: ISPOR 2024; May 7-10 2023; Boston, USA. Value Health. 2023;26(6 Suppl):S98. https://www.valueinhealthjournal.com/article/S1098-3015(23)00617-4/abstract
10. Breslau RM, Cohen JT, Diaz J, Malcolm B, Neumann PJ. A review of HTA guidelines on societal and novel value elements. Int J Technol Assess Health Care. 2023;39(1):e31. doi:https://doi.org/10.1017/s026646232300017x

