From Health to Well-Being: Toward a Monetary Valuation of a Well-Being Adjusted Life-Year
Brinkmann C, Stargardt T, Brouwer WBF. Value Health. 2024;27(7):857-870.
Section Editor: Agnes Benedict
Health-related quality of life and quality-adjusted life-year (QALY) has been the standard measure in economic evaluations and is now used widely in many countries for health technology assessment decision making. A broader concept, that of well-being, goes beyond health. Well-being has many different definitions, but a common one is that used in the ICECAP-A (the ICEpop CAPability measure for Adults tool,) focusing on domains, such as stability (ability to feel settled), attachment (ability to have love/ friendship and support), autonomy (ability to be independent), achievement (ability to achieve progress in life), and enjoyment (ability to experience enjoyment and pleasure) has been proposed and empirically measured using a variety of measures.
To aid decision making regarding resource allocations, the use of well-being-adjusted life years, or WALYs, similarly to QALYs, require an assessment of how much one unit of WALY is worth for society. This is the subject of the paper by Brinkmann, Stargardt, and Brouwer presented based on results of a large contingent valuation exercise, as part of the 11th and final wave of the European COVID Survey. Data were gathered from representative cross-sectional samples, with approximately 1000 adults from each of the following countries: Denmark, France, Germany, Italy, The Netherlands, Spain, and the United Kingdom, between November-December 2022.
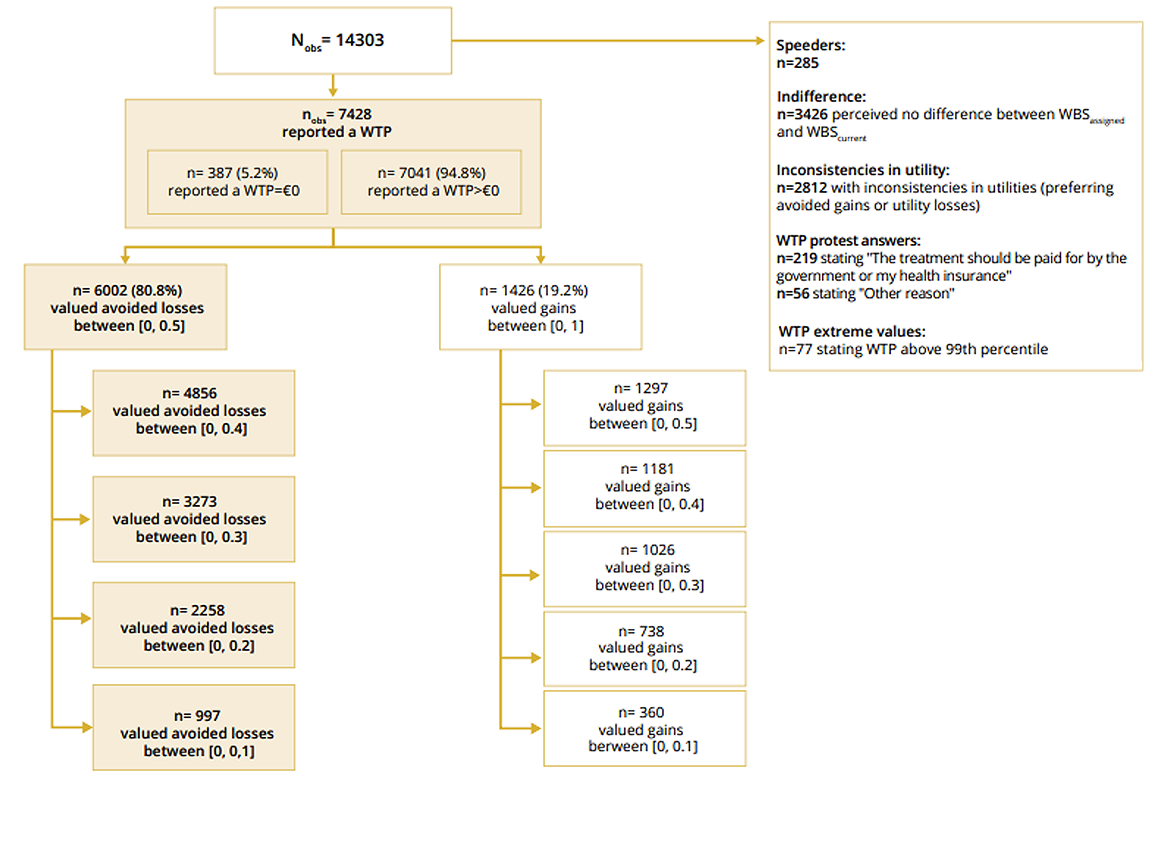
Valuations were done on changes in well-being relative to participants’ current well-being score, using hypothetical examples. Participants were divided into 2 groups (see Figure). If a participant expressed a preference for the assigned well-being score over their current one, the participant was asked to imagine the opportunity to purchase a treatment that is approved, painless, and without side effects, that would get them to the assigned well-being state for a duration of 1 month. Vice versa, if the participant preferred their current well-being state over the assigned one, the participant was asked to imagine a sudden event that would lead to a loss of well-being to the assigned well-being state for 1 month and were told about a treatment that can prevent the loss. Their willingness to pay to access the treatment was explored. Full details of the methods are described in the paper.
Researchers restricted their analytical datasets to responses that were consistent, excluded participants doing the exercise too rapidly; made adjustments for cross-country differences in purchasing power, and took into account patients’ different demographic and socioeconomic status (see Figure).
Figure. Sample flow chart.
The authors found that only willingness to avoid the loss was consistent with expected behavior. Their main results suggest that a WALY may be valued as little at €13,000 or as high as €61,000 across the European population, depending on the specific change that was being valued. Smaller incremental changes traded off resulted in much higher willingness-to-pay values than large ones. Notably, the authors present a large set of subgroup specific results and regression analyses, providing a very good insight to the reader regarding the country-specific data and variability in individual preferences.
The paper is special in that it lists a very comprehensive set of limitations and inconsistencies transparently, pointing out issues with the methods of data capture, as well as potential reasons for their very variable findings. They acknowledge that this is a crude first attempt at quantifying the value of a WALY, using one specific instrument. Nevertheless, this study investigates less-explored but very important dimensions of quality of life that complements health-related aspects of quality of life, which can then provide guidance to resource allocation toward both nonhealth and healthcare interventions.

