Development of a Value-Based Payment Model for Patients With Osteoarthritis for the Bulgarian Healthcare System
Yoanna Vutova, MPharm, HTA Ltd, Sofia, Bulgaria; Slaveyko Djambazov, PhD, Plamen Kinov, PhD, DSc, Georgi Lukanov, BS, ORFIO, Sofia, Bulgaria
Hip and knee osteoarthritis (OA) represents a significant global health challenge, affecting millions of individuals and leading to considerable disability and financial burden on healthcare systems worldwide. This chronic condition necessitates long-term management strategies, including surgical interventions such as arthroplasty, to alleviate pain and restore function. However, the increasing OA prevalence, coupled with rising life expectancies, is anticipated to further escalate the demand for these costly surgical treatments, which poses a substantial economic challenge.
In Bulgaria, the current stage of OA management involves significant waiting times for surgical procedures and varying rates of complications. Outcome assessment measures, such as the time to procedure and postsurgical complications, are tracked but not consistently integrated into a comprehensive quality-improvement framework. Although a local registry was established in 2022, it is not used consistently and could not serve as a reliable database for complication rates or performance measurement.
Current healthcare payment models, particularly fee-for-service, prioritize the quantity of care over the quality of outcomes achieved. This model incentivizes healthcare providers to increase the volume of services without measuring improvements in patient outcomes. As a result, patients may receive unnecessary treatments and experience avoidable complications contributing to inefficiencies, variable care quality, and increased healthcare spending.
"In Bulgaria, the current stage of OA management involves significant waiting times for surgical procedures and varying rates of complications. Outcome assessment measures are tracked but not consistently integrated into a comprehensive quality-improvement framework."
Recognizing the urgent need for reform, a team of value-based healthcare experts in collaboration with ORFIO, a prominent orthopedic nongovernmental organization with leading orthopedists, is poised to enact transformative change in Bulgaria’s healthcare system. Our initiative targets the financial burdens and quality gaps inherent in OA treatment through the introduction of an innovative payment model for hip and knee arthroplasty. Our proposed solution involves the implementation of a bundle payment, designed to encompass the entire spectrum of OA care—from initial consultations to postoperative rehabilitation, inclusive of the most common complications.
The bundle payment model offers significant value for all stakeholders. For the payer (ie, National Health Insurance Fund [NHIF]), it provides a predictable cost structure and aligns payments with the quality of care, aiming to reduce overall healthcare spending by minimizing complications and unnecessary procedures. For the provider, it incentivizes the delivery of high-quality coordinated care, leading to better patient outcomes and potentially higher reimbursement rates linked to performance metrics. For the patient, value-based perspectives maximize outcomes, ensuring that care focuses on achieving the best possible health results rather than simply reducing costs.
Research and Results
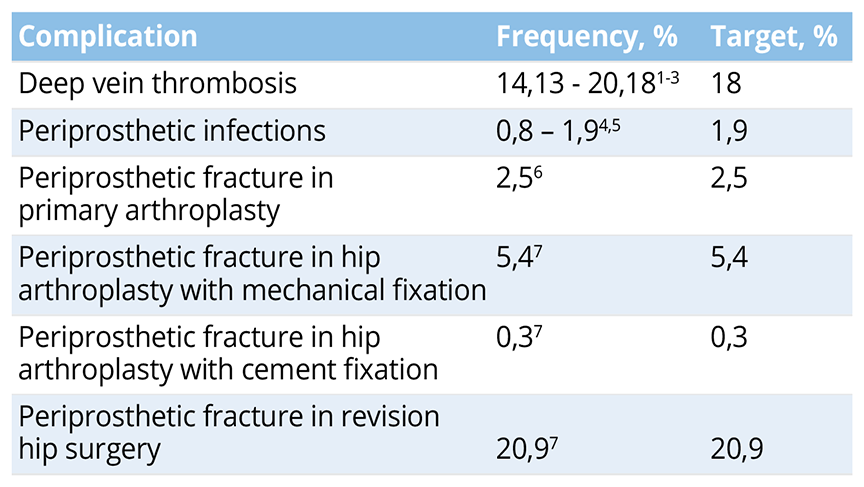
The bundle payment covers the entire treatment cycle for patients with hip and knee OA undergoing joint alloplasty, including preoperative care, diagnostic imaging, hospitalization (excluding prosthesis), 3-month follow-up, treatment of the most common complications, and 14-day rehabilitation in the bundle price. Table 1 outlines the most common complications, respective frequencies, and target percentages associated with total knee and hip arthroplasty procedures included in the bundle price. The frequencies represent the expected occurrence of complications based on current data, while the target percentages indicate the desired reduction in complication rates following the completion of the 1-year pilot phase. The objective of the pilot phase is to establish an environment conducive to enhancing outcomes, promoting care integration, and encompassing the entirety of the care cycle. Therefore, some of the target values in Table 1 are intentionally set to be achievable.
Table 1. Complication rate target for patients with OA undergoing surgical treatment.
The current practice involves fragmented care with separate billing for each service, leading to inefficiencies and higher costs. The new management pathway integrates all aspects of OA care into a single bundled payment, encouraging coordinated care and resource utilization. The bundle payment approach encourages healthcare providers to minimize complications, thereby reducing the additional costs associated with postoperative complications and inefficient treatment strategies, leading to an increase in overall value.
"The bundle payment approach encourages healthcare providers to minimize complications, thereby reducing the additional costs associated with postoperative complications and inefficient treatment strategies, leading to an increase in overall value."
To prevent selective bias, the program is risk-stratified and includes only healthy patients or patients with a minor medical condition undergoing surgical treatment, as defined by the American Society of Anesthesiologists (ASA) classification - ASA I and ASA II. Nonplanned events, such as unexpected complications or additional treatments, are incorporated into the payment scheme by setting aside a contingency fund within the bundle. The exclusion of prostheses is based on the variability in prosthesis choice and cost. This aspect will be reviewed and potentially included in future iterations of the bundle payment model based on feedback from the pilot phase.
Six Bulgarian hospitals will participate voluntarily for 1 year. At the end of the pilot phase, the program will be evaluated based on the feedback of the medical institutions that have participated and on an effectiveness analysis. The evaluation should determine whether the implementation of the program has led to improvements in clinical and important patient outcomes, whether other facilities will be included, or whether changes and adjustments are needed to achieve the objectives.
Key expectations include:
- Improved patient outcomes, including reduced complication rates and enhanced quality of life
- Cost savings for the healthcare system due to reduced complications and more efficient care delivery
- Increased provider engagement and satisfaction through aligned incentives and streamlined care processes
Limitations include:
- Initial resistance from providers accustomed to fee-for-service models
- Challenges in data integration and interoperability between different IT systems
- Need for comprehensive change management strategies to support the transition
- Long-term sustainability and scalability of the value-based payment model require further investigation
The outcome measurement is facilitated through the utilization of Bulgaria’s arthroplasty register inaugurated in 2022. This resource is freely accessible to voluntary clinics participating in the initiative. The research methodology leveraged the Institutional Consortium for Health Outcomes Measurement standardized set for hip and knee OA treatments, encompassing a suite of measures that includes administrative, clinical, and patient-reported data.8 Patient-reported outcome measures are regularly assessed through an innovative online messaging tool designed to streamline data collection and enhance patient engagement.
The stakeholders involved encompass a diverse range of actors, each playing a crucial role in the success of the initiative, including ORFIO, HTA Ltd team of value-based healthcare experts, healthcare facilities and providers, government agencies, NHIF, patients, and technology providers. All stakeholders collaborate and contribute to ensure the successful implementation and sustainability of bundle payments for patients with OA.
For the successful implementation of bundle payments for patients with OA in Bulgaria, a regulatory amendment will be made in the National Framework agreement between the NHIF and the Bulgarian Medical Union, which involves the establishment of a new clinical pathway tailored specifically to accommodate the requirements and protocols of the bundle payment model. This new clinical pathway encompasses guidelines, protocols, and standards of care designed to optimize the delivery of healthcare services within the framework of bundle payments. It outlines the sequential steps involved in the assessment, treatment, and management of patients with OA, ensuring consistency, efficiency, and quality throughout the care continuum.
Lessons Learned
The lessons learned through the development of the pilot program offer valuable guidelines for implementing such transformative healthcare models.
1. Utilizing standard sets proved instrumental in ensuring a consistent and meaningful assessment of treatment efficacy. This approach underscores the importance of standardized outcome measures in driving improvements in patient care and should be considered a best practice in healthcare reforms.
2. The adoption of bundle payments highlights several benefits, including fostering a more collaborative approach and encouraging innovation in care delivery to maximize efficiency and effectiveness. This model promotes a holistic view of patient care, aligning financial incentives with the achievement of positive patient outcomes. Incentivization stems from the fact that if it is not present, providers will bear the cost of treating complications.
3. Engaging healthcare providers and explaining the mutual benefits of the value-based payment model is crucial for its acceptance and success. Education and transparent communication about the goals and mechanics of the model facilitate buy-in from practitioners and administrative staff, showcasing the importance of stakeholder engagement in healthcare initiatives.
Challenges and Areas for Improvement
1. While the division of roles within medical facilities for data collection optimizes the process, integrating these data into a cohesive and actionable format poses challenges.
2. Transitioning to a value-based model requires significant changes in organizational culture and processes. Initial resistance from providers accustomed to the fee-for-service model is a notable challenge.
3. While the pilot program provides encouraging results, the long-term sustainability and scalability of the value-based payment model require further investigation.
4. The voluntary nature of the program’s participation highlights the difficulty in achieving a critical mass of participating facilities. Moving forward, strategies to incentivize participation or demonstrate the value proposition of such models more clearly could help in overcoming this barrier.
"For the successful implementation of bundle payments for patients with OA in Bulgaria, a regulatory amendment will be made in the National Framework agreement between the NHIF and the Bulgarian Medical Union, which involves the establishment of a new clinical pathway tailored specifically to accommodate the requirements and protocols of the bundle payment model."
The implementation of a value-based payment model for OA treatment offers profound lessons for healthcare reform efforts. Best practices, such as focusing on outcome measurement, utilizing bundle payments, and engaging stakeholders are key drivers of success. However, addressing challenges related to data integration, managing the transition, and ensuring long-term sustainability is essential for the model’s future adoption and impact.
References
1. Kawai T, Goto K, Kuroda Y, Matsuda S. Lower activity and function scores are associated with a higher risk of preoperative deep venous thrombosis in patients undergoing total hip arthroplasty. J Clin Med. 2020;9(5):1257.
2. Santana D, Emara A, Orr M, et al. An update on venous thromboembolism rates and prophylaxis in hip and knee arthroplasty in 2020. Medicina. 2020;56(9):416.
3. Wainwright T, Burgess L, Middleton R. A single-centre feasibility randomised controlled trial comparing the incidence of asymptomatic and symptomatic deep vein thrombosis between a neuromuscular electrostimulation device and thromboembolism deterrent stockings in post-operative patients recovering from elective total hip replacement surgery. Surg Technol Int. 2020;36:289-298.
4. Kamath A, Ong K, Lau E. Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplasty. 2015;30(9):1492-1497.
5. Bjerke-Kroll B, Christ A, McLawhorn A. Periprosthetic joint infections treated with two-stage revision over 14 years: an evolving microbiology profile. J Arthroplasty. 2014;29(5):877-882.
6. Konan S. Periprosthetic fractures associated with total knee arthroplasty: an update. Bone Joint J. 2016;98-B(1):1489-96.
7. Berry D. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30(2):183-190.
8. Rolfson О, Wissig S, van Maasakkers L, et al. Defining an international standard set of outcome measures for patients with hip or knee osteoarthritis: consensus of the International Consortium for Health Outcomes Measurement Hip and Knee Osteoarthritis Working Group. Arthritis Care Res. 2016;68(11):1631-1639.

