The Health ROI Assessor: Evaluating Novel CVD Prevention Approaches in Estonia
Karla Hernandez-Villafuerte, PhD; Maike Schmitt, PhD; Jan Ludwig Fries, PhD, WifOR Institute, Darmstadt, Hessen, Germany
Introduction
Substantial evidence supports the link between improved health, economic growth, and well-being across countries.1-6 However, there’s been limited progress in advocating for increased national budget allocation to the health sector because, despite the evidence, health investments have been viewed historically as an economic burden rather than a driver of growth. The absence of empirical evidence on the pathway that links a particular investment in health and the resulting economic growth and a lack of frameworks and metrics estimating return on investment (ROI) contribute to this challenge.
Concern arises when health investments, such as those related to population prevention programs, demand a significant portion of the health sector budget. In such cases, policymakers grapple with limited budgets and imperfect information. The current health technology assessment (HTA) tools, primarily designed for curative care, inadequately capture the value for money in preventive measures like screening or vaccination, adding to the difficulty.7-9
In light of recent economic challenges stemming from the COVID-19 pandemic, there’s a renewed interest in understanding how health investments contribute to economic growth and stability. Current research highlights 3 main mechanisms: first, health investments drive innovation for better disease management, reducing healthcare costs.10-14 Second, a healthier population is more productive.3,4,12,14 Third, health investments impact the broader economy by influencing supply and demand across sectors.15,16 Despite these insights, there’s a lack of consistent efforts to predict the total ROI of health expenditures holistically, leaving current research results on rhetorical explanations with limited use in informing policy decisions.
We propose an innovative approach entailing a societal and macroeconomic perspective to assess value creation of health investments promoting countries’ economic growth: the Health ROI Assessor framework that we operationalize in a measurement tool. This study applies the Health ROI Assessor for the first time to evaluate the ROI of a real-world prevention program in Estonia, proposed by the Prevent Cardiovascular Disease Coalition (P-CVD). We assessed the value creation of health investments reducing cardiovascular disease (CVD) burden and promoting economic growth within the country. Estonia has one of the highest CVD event rates in Europe and a comparatively high prevalence of CVD risk factors, which lead to high direct and indirect costs.17,18 In 2019, CVD accounted for over 50% of adult mortality and over 38,000 hospitalization cases.* The P-CVD program provides a tailored solution to reduce low-density lipoprotein cholesterol (LDL-C), where CVD event risk profiles consider the cumulative exposure to LDL-C of the considered population (males/females, ages 30-79 years, without CVD history).
Methodology
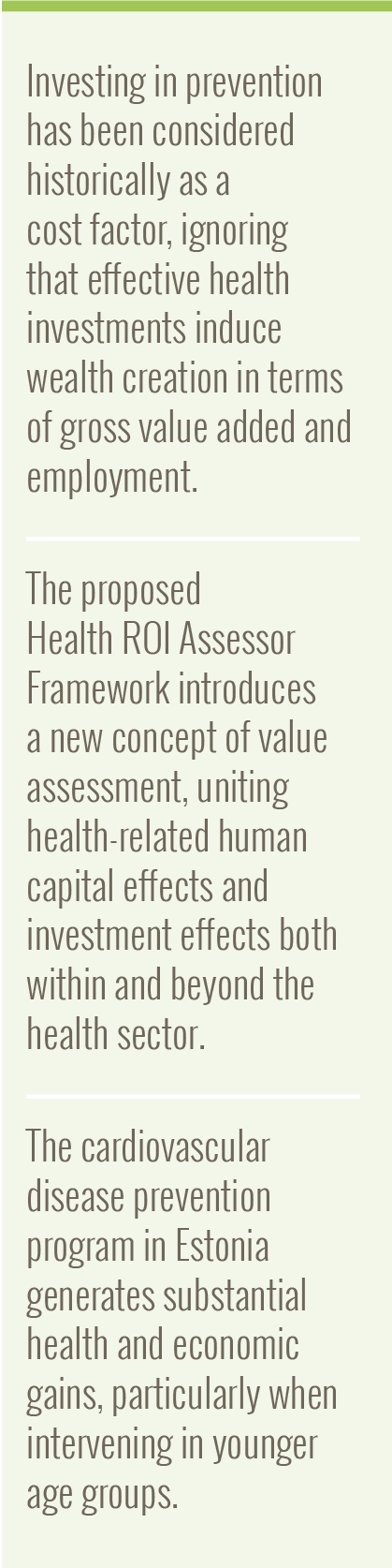
The framework includes 2 pillars (Figure 1): The Health Economy (HE) Footprint estimates direct effects within the HE (gross value added [GVA] and corresponding job creation) and spillovers to other economic sectors (indirect/induced effects). The analysis builds on multiregion input–output data, tracing the value chain of health throughout economies19-21 to estimate the magnitude of the health sector. The Human Capital Effect evaluates gains in productivity related to better health outcomes, incorporating paid and unpaid work participation. Labor-market interactions connect both pillars via labor-force supply/demand adjustments.
Figure 1. Health ROI Assessor framework
Model inputs include age-, gender- and risk-specific previously estimated avoided CV events based on the results of a cost-effectiveness model implemented in a separate project.22 Time series analysis allows us to build a dynamic framework of health investments. The implementation is based on health and economic data from official statistics and considers a discount rate of 3.5%.
We evaluated 2 scenarios: the base case scenario assesses short-term impacts over 15 years, and an alternative scenario examining long-term effects on the population initiating the P-CVD program in the 30-39 years of age cohort. The latter scenario focuses on the human capital pillar, extending to an estimated productive life expectancy of 85 years. Furthermore, it assumes that economic variables will remain constant beyond the initial 15 years, mirroring values predicted in the latest forecasted year.
Results
Base case scenario – Short-term effects
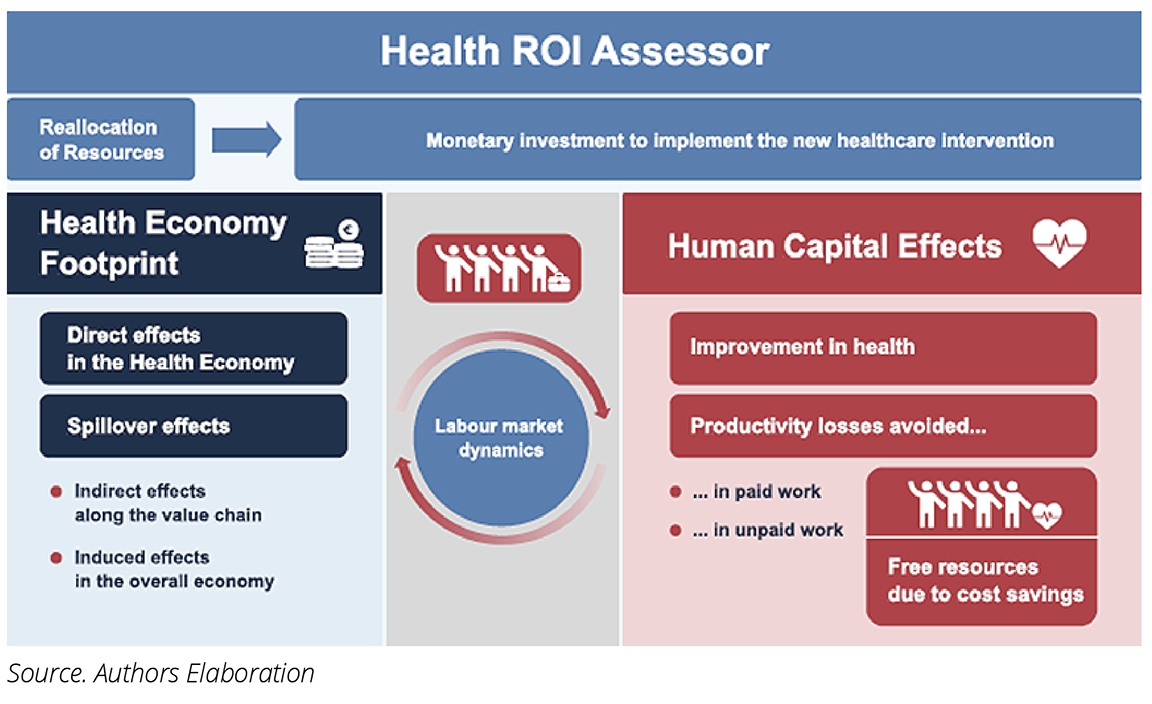
Results illustrate considerable ROIs from the P-CVD program. For the HE Footprint (Figure 2), we assume a value of €20 million additional funding into the health system to implement the intervention, distributed equally over 5 years. This capital injection induces €46 million GVA and 1177 additional jobs in direct, indirect, and induced effects over 10 years.
Figure 2. Short-term: Cumulative value created in HE Footprint pillar (first 15 years)
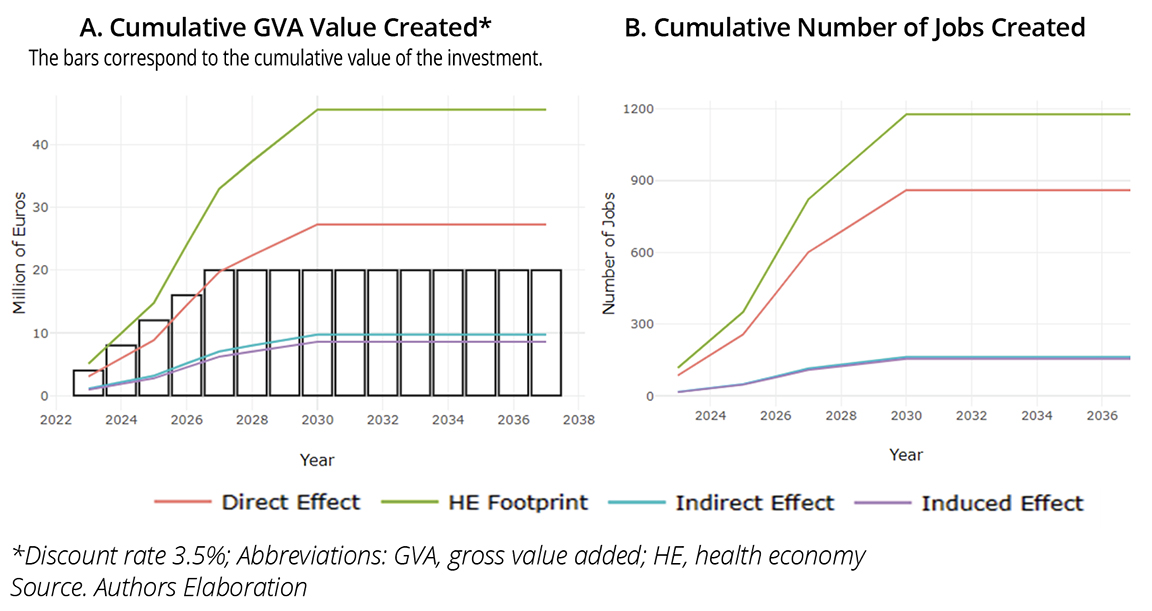
Regarding the Human Capital Effects, for a population of 50,527 individuals participating in the P-CVD program, P-CVD prevents 315 deaths and 928 nonfatal events over 15 years. This translates to an increase in paid (€47.97 million) and unpaid work (€61.20 million) productivity of €109.18 million. Given higher CVD incidence in older age cohorts, the short-term CV events avoided are less for younger cohorts. Therefore, the highest paid work productivity gains occur for the 50-69 years of age cohorts (Figure 3A). Additionally, Figure 3B displays that the differences in unpaid work productivity gains are more pronounced between the older and younger age cohorts than those observed in Figure 3A, reflecting varying time utilization patterns.
Figure 3. Short-term: Cumulative value created** by age cohort in the Human Capital Effects pillar (first 15 years)
Alternative scenario – Long-term effects resulting from the Human Capital Effects pillar
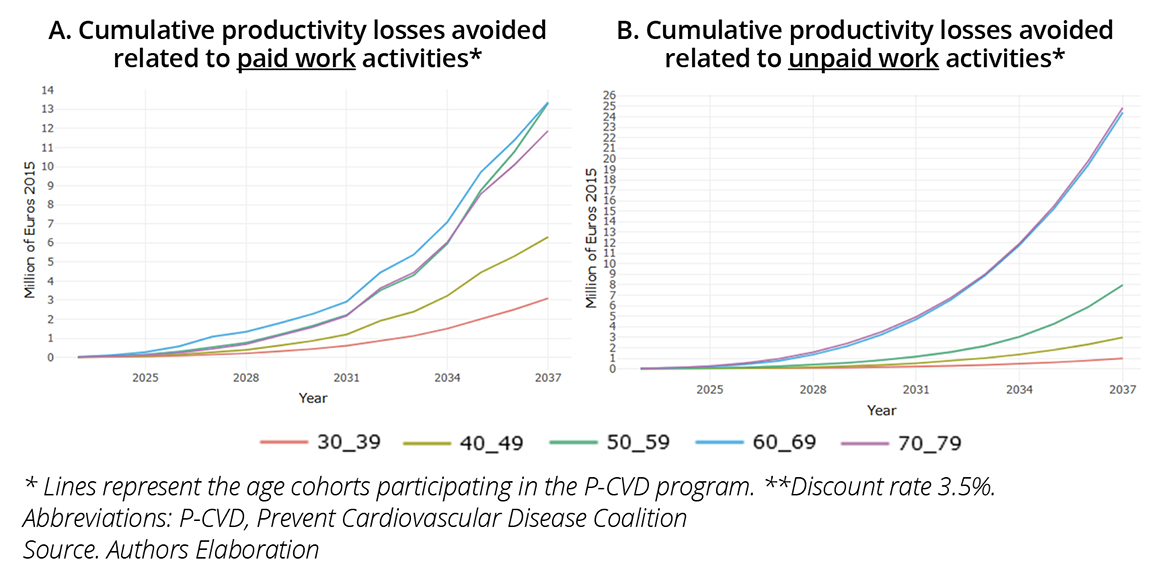
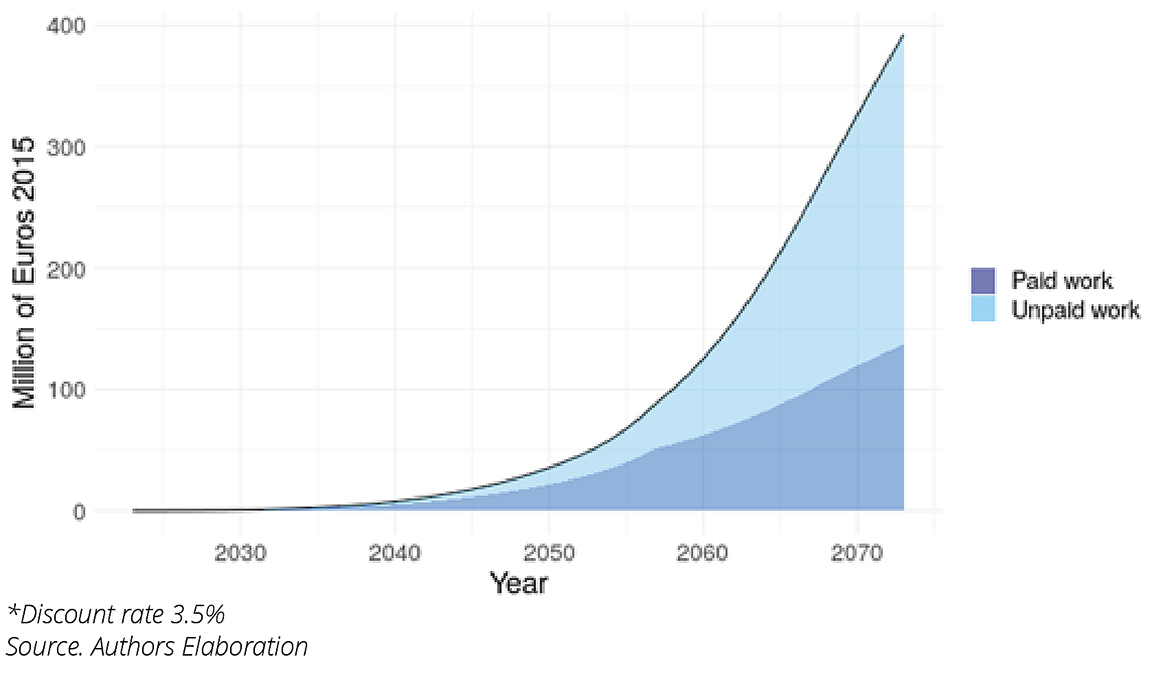
Assuming a maximum productive lifespan of 85 years, enrolling a cohort of 12,077 individuals aged 30–39 in the P-CVD program results in a gain of 13.35 million productive hours. It translates into €392.35 million of value creation (GVA), where the majority corresponds to productivity gains in unpaid work (Figure 4).
Figure 4. Long-term: Cumulative value created* in the 30 to 39 years of age cohort along their productive lifespan
Discussion
The Health ROI Assessor framework is the first to offer a comprehensive perspective on the overall value of healthcare intervention programs, complementing conventional economic evaluations. This is particularly crucial for impactful interventions with substantial investments. For example, prevention programs yield long-term benefits by contributing to human capital formation and creating a cascade of effects that start in the health sector and affect the entire economy.
Results suggest a substantial economic impact of implementing the P-CVD program in Estonia, even in the short-term (first 15 years). The HE Footprint pillar suggests a ROI in terms of GVA contribution equal to 2.3 times the amount invested in the P-CVD program when capturing effects along the entire value chain. The Human Capital Effect indicates an increase in productivity of €109 million, which corresponds to around 0.4% of Estonia’s GDP in 2023 (2015 prices).
While short-term productivity gains in younger populations are modest, the long-term cumulative impact is significant. The youngest cohort (30-39 years old) experiences a reduction in CVD events that results in €392 million productivity gains, equivalent to 1.6% of Estonia’s GDP in 2023 (2015 prices). This underscores the economic value of investing in early prevention, especially targeting younger age groups, for sustained long-term growth.
The proposed framework offers key advantages. It links macroeconomic investment perspectives with microeconomic social impact evaluations, providing a holistic view of improved population health. Unlike traditional methods, we monetize using sector-specific GVA per working hour instead of wages, enhancing the accuracy in reflecting the value of labor productivity. By using national accountability data and publicly available economic variables, our results can be integrated into a country’s accounting system. Furthermore, the methodology’s adaptability makes it applicable to diverse countries and healthcare interventions, facilitating comparisons and evaluations. The Human Capital Formation addresses the impact of a healthier population, emphasizing productivity as a key factor.
This is crucial to counter the alarming decline in the percentage of individuals in the working-age population, which represents a substantial threat to future financial and fiscal sustainability.23-27 Additionally, the capacity for unpaid work, an often-overlooked aspect crucial for economic well-being and societal health, is considered. Unpaid work is estimated to exceed 40% of GDP in some countries,28 disproportionately affecting women’s participation in the paid economy29 and constituting a significant component of older adults’ contributions to economic growth.30 Finally, by considering input–output methods, our framework allows policymakers to compare the healthcare and other economic sectors in terms of the economic gains of injecting capital into the system.
The initial version of the Health ROI Assessor has limitations typical of a first modeling attempt, which will be captured in an enhanced version in development. First, predictions rely on available data and applied assumptions. Second, while it addresses relevant macroeconomic and societal effects, some aspects, such as the productivity of informal caregivers, are not included. Third, direct cost savings in the healthcare system from reduced treatment demand are not factored in. However, this dimension has been addressed in the work of Clayson et al.22 For the intervention program under consideration, they report a total direct cost reduction of €323,757 per 1000 individuals, which is roughly 51%. In a future version of the ROI Assessor framework, we intend to incorporate these gained resources in an additional stream of value creation.
Conclusion
Results suggest substantial economic effects of implementing the P-CVD program in Estonia. The highest accumulative economic value creation is achieved when the intervention affects populations at younger ages.
The Health ROI Assessor framework offers an innovative approach to simultaneously evaluate the human capital and economic effects of healthcare interventions. Aligned with the G20 partnership for health and development’s call for a more structured approach to health investment assessment, our framework addresses this need. Amid ongoing global challenges, our tool stands out as a valuable addition to economic evaluation tools, aiding policymakers in optimizing resource allocation for enhanced population well-being. Shifting from a cost-centric viewpoint, the framework contributes to an understanding of public health and related interventions as a motor of economic and societal growth.
Acknowledgements
We gratefully acknowledge valuable discussion and comments during the conduct of the study from Dennis A. Ostwald (Founder and CEO, WifOR Institute), Rifat Atun (Professor of Global Health Systems and Director, Health Systems Innovation Lab, Harvard University), Mark Sculpher (Professor and Director of the Centre for Health Economics, University of York), and Andrew Bushell, who initiated the Prevent CVD program (Global Program Head, Novartis). We further want to thank the close collaboration with Amaris consulting, who provided the results of the cost-effectiveness analysis.
Data Availability
Data provided by the Estonian National Institute for Health Development (NIHD /TAI) upon request. Detailed methodology for the Health ROI Assessor is available upon request.
References
- Preston SH. The changing relation between mortality and level of economic development. Population Studies. 1975;29(2):231-248.
- Sachs JD, Ahluwalia IJ, Amoako KY, et al. Investing in health for economic development: Scaling up response to infectious diseases. Weltgesundheitsorganisation, ed. Geneva: World Health Organization; 2001.
- Suhrcke M, McKee M, Stuckler D, Sauto Arce R, Tsolova S, Mortensen J. The contribution of health to the economy in the European Union. Public Health. 2006;120(11):994-1001.
- Jamison DT, Summers LH, Alleyne G, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382(9908):1898-1955.
- Bloom DE, Kuhn M, Prettner K. Health and Economic Growth. IZA Institute of Labor Economics. https://docs.iza.org/dp11939.pdf. Published November 2018.Accessed March 2023.
- Bloom D, Canning D, Sevilla J. The Effect of Health on Economic Growth: Theory and Evidence. National Bureau of Economic Research. http://www.nber.org/papers/w8587.pdf. Published November 2001. Accessed March 2023.
- Haacker M, Hallett TB, Atun R. On discount rates for economic evaluations in global health. Health Policy Plan. 2020;35(1):107-114.
- Bos JM, Beutels P, Annemans L, Postma MJ. Valuing prevention through economic evaluation. Pharmacoeconomics. 2004;22(18):1171-1179.
- Jit M, Mibei W. Discounting in the evaluation of the cost-effectiveness of a vaccination programme: a critical review. Vaccine. 2015;33(32):3788-3794.
- Civan A, Köksal B. The effect of newer drugs on health spending: do they really Increase the costs? Health Economics. 2010;19(5):581-595.
- Cutler DM, McClellan M. Is technological change in medicine worth it? Health Affairs. 2001;20(5):11-29.
- Lichtenberg FR. Are the benefits of newer drugs worth their cost? Evidence from the 1996 MEPS. Health Affairs. 2001;20(5):241-251.
- Lichtenberg FR. The impact of new drugs on US longevity and medical expenditure, 1990–2003: evidence from longitudinal, disease-level data. American Economic Review. 2007;97(2):438-443.
- Zozaya N, Alcalá B, Galindo J. The offset effect of pharmaceutical innovation: a review study. Glob Reg Health Technol Assess. 2019;2019:1-10.
- Chen Q, Wei HM, Zhi YP. The impact of health investment on industrial structure: “spillover” or “crowding out”?—evidence from emerging market countries. Front Public Health. 2022;9:1-13.
- Pereira AM, Pereira RM, Rodrigues PG. Health care investments and economic performance in Portugal: an industry level analysis. Journal of Economic Studies. 2019;46(6):1174-1200.
- Timmis A, Vardas P, Townsend N, et al. European Society of Cardiology: cardiovascular disease statistics 2021. Eur Heart J. 2022;43(8):716-799.
- Kaldmäe M, Zemtsovskaja G, Abina J, Land T, Viigimaa M. Prevalence of cardiovascular disease risk factors in Tallinn, Estonia. Medicina. 2017;53(4):268-276.
- World Input-Output Database. University of Groningen. https://www.rug.nl/ggdc/valuechain/wiod/. Updated September 18, 2024. Accessed March 2023.
- The Eora Global Supply Chain Database. World MRIO. https://worldmrio.com/. Accessed December 2022.
- Lenzen M, Moran D, Kanemoto K, Geschke A. Building EORA: a global multi-region input–output database at high country and sector resolution. Economic Systems Research. 2013;25(1):20-49.
- Clayson M, Gauthier A, Grustam AS, Viigimaa M, Sculpher M. Using a cumulative low-density lipoprotein cholesterol modelling approach to estimate the reduction of risk of atherosclerotic cardiovascular events from a primary prevention program. Value Health. 2023;26(12):S79–80.
- Ageing Europe - statistics on population developments. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_statistics_on_population_developments. Published 2020. Accessed February 2023.
- Maestas N, Mullen KJ, Powell D. The effect of population aging on economic growth, the labor force, and productivity. Am Econ J Microecon. 2023;15(2):306-332.
- Leaving no one behind in an ageing world: World Social Report 2023. United Nations Department of Economic and Social Affairs. https://desapublications.un.org/file/1087/download. Published 2023. Accessed February 2023.
- Bloom DE, Canning D, Fink G. Implications of population ageing for economic growth. Oxf Rev Econ. 2010;26(4):583-612.
- Peng D, Fei W. Productive ageing in China: development of concepts and policy practice. Ageing Int. 2013;38(1):4-14.
- Why measuring unpaid domestic and care work matters, and how we can help.. International Labour Organization (ILOSTAT). https://ilostat.ilo.org/topics/unpaid-work/measuring-unpaid-domestic-and-care-work/. Accessed March 2023.
- Ferrant G, Pesando LM, Nowacka K. Unpaid care work: the missing link in the analysis of gender gaps in labour outcomes. OECD Development Centre. https://www.oecd.org/dev/development-gender/Unpaid_care_work.pdf. Published December 1, 2014. Accessed March 2023.
- Bloom DE, Khoury A, Algur E, Sevilla JP. Valuing productive non-market activities of older adults in Europe and the US. De Economist. 2020;168(2):153-181.

