Pharmacoeconomic Guidelines: South Africa
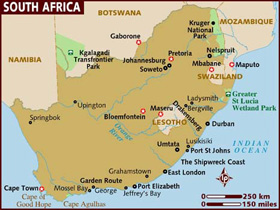
Country/Region: South Africa
Published PE Recommendations
Guidelines for Pharmacoeconomic Evaluations of Medicines and Scheduled Substances (February 2013)
PDF in English
Information current as of Wednesday, January 17, 2018
Key Features
| Key Features | |
|---|---|
| Type of Guidelines | Published PE Recommendations |
| Title and year of the document | Guidelines for Pharmacoeconomic Submissions (December 2012) |
| Affiliation of authors | National Department of Health |
| Purpose of the document | To describe the process to be followed for PE applications and the criteria for medicines which require submissions; To create a forum which provides independent and objective review of the value of medicines |
| Standard reporting format included | Yes |
| Disclosure | Nothing required |
| Target audience of funding/ author's interests | Pharmaceutical companies, researchers, decision makers |
| Perspective | Default perspective: third-party payer. Option to use a broader perspective where justified according to specific considerations. |
| Indication | Approved Indication |
| Target population | If submission pertains to a specific sub-group, within the registered indication, this must be clearly defined |
| Subgroup analysis | Yes (only if the group has been defined a priori in the clinical trial protocol and the study was sufficiently powered to analyse specified strata. |
| Choice of comparator | The main comparator is deemed to be the standard of care for local practice. All possible comparators need to be listed and justified. |
| Time horizon | Time Horizon is based on the natural course of the condition and the likely impact of the treatment. Depending on the type of intervention, it may be necessary to present a short term analysis based on the primary clinical data. |
| Assumptions required | Yes |
| Preferred analytical technique | Any of CMA, CEA, CUA and CBA considered but choice of analysis must be clearly justified. The modelled evaluation should be based on the outcomes measures which most closely validly estimate the final outcome. |
| Costs to be included | Direct costs. Indirect costs should generally be excluded. |
| Source of costs | No prefered source specified, although table needs to be provided clearly identifying the source of the reference for unit costs. |
| Modeling | Yes - where randomised trials available do not provide sufficient information. Modelling options include spreadsheet analysis, decision analysis, Markov models and Monte Carlo simulations. |
| Systematic review of evidences | Yes, including crtieria for inclusion and exclusion of sources of evidence, evaluation of clinical trials for inclusion, assessment of measures taken to minimize bias, meta-analysis and indirect comparison. Searhc strategy to be clearly defined and be reproducible. |
| Preference for effectiveness over efficacy | Yes. |
| Preferred outcome measure | Life Years Gained, deaths prevented or QALYs gained |
| Preferred method to derive utility | No preference stated for measurement of utilities |
| Equity issues stated | No differentiation between QALYs accruing to different groups |
| Discounting costs | Future costs should be discounted at an annual rate of 5% (range 0% to 10% for sensitivity analysis) |
| Discounting outcomes | Future benefits should be discounted at an annual rate of 5% (range 0% to 10% for sensitivity analysis) |
| Sensitivity analysis-parameters and range | Sensitivity analysis must be conducted on all variables using an appropriate range, as justified and referenced. Results to be presented in tabular form and tornado diagrams. |
| Sensitivity analysis-methods | One way sensitivity analysis must be conducted on all variables using an appropriate range, as justified and referenced. Two-way sensitivity analysis should be conducted on variables shown to be sensitive in the one-way analysis. |
| Presenting results | Results to be presented in a disaggregated form, and then increasingly aggregated. Present appropriately aggregated and discounted costs results separately for outcomes and resources and separtely for proposed medicine and its comparator. The final outcome should be presented as an ICER. |
| Incremental analysis | Yes |
| Total costs vs effectiveness (cost/effectiveness ratio) | Yes |
| Portability of results (Generalizability) | The patient population to which the pharmacoeconomic evaluation applies should be consistent with the patient population defined in the clinical part of the reimbursement request submission. |
| Financial impact analysis | Not specified |
| Mandatory or recommended or voluntary | Currently, the submission for pharmacoeconomic assessment is essentially voluntary, however, key figures in the Department of Health have to power to "call a product up" for economic assessment. |
Acknowledgement: