Multistakeholder Healthcare Cooperatives: A New Paradigm for Healthcare Delivery in India
Narendra Javadekar, MD, DNB, MA, Maharashtra Medical Research Society and Gokhale Institute of Politics and Economics, Pune, India; Archana Javadekar, MD, DNB, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pune India; Geeta Pardeshi, MD, MSc, MPH, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, India; Sanjay Juvekar, PhD, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pune, India
Background
India is home to a fifth of the world’s population. Socioeconomic transition, rapid urbanization, aging population, and climate change make India home to a significant burden of the communicable and noncommunicable diseases.1 The complex healthcare system in India is resource constrained and is focused on curative aspects, and using technology makes it even more expensive. This drives vulnerable families below the poverty line due to catastrophic out-of-pocket health expenditures.2 About 70% of people seek healthcare primarily from out-of-pocket expenditure, 10% from insurance, and nearly 20% from the government health system that majorly serves people from lower socioeconomic strata. This percentage is expected to rise to 40% under the coveted Ayushman Bharat Scheme.3 Heightened expectations and market-oriented healthcare delivery often result in frustration among patients’ families, causing occasional incidents of violence against doctors and hospitals.4
As the problems are at the system level, so must be the solutions. To achieve universal health coverage by 2030, solutions such as nationalization of the healthcare system or encompassing the whole and diverse country into the folds of insurance are almost impossible. Including the private sector in national health programs is not an easy solution either. Can systems engineering give us an answer?
System analysis of healthcare delivery
Healthcare systems are shaped by inherent philosophies and religious backgrounds. But values such as justice, human dignity, and caring for people who need help are common to all. These values, embodied in Hippocratic oath and World Medical Association’s declarations, indicate the need for people to be able to care of and make decisions about their health.5 It is necessary to base the healthcare system on the rules that protect these values and empower people to be self-reliant in health matters ensuring contextual synchronization.
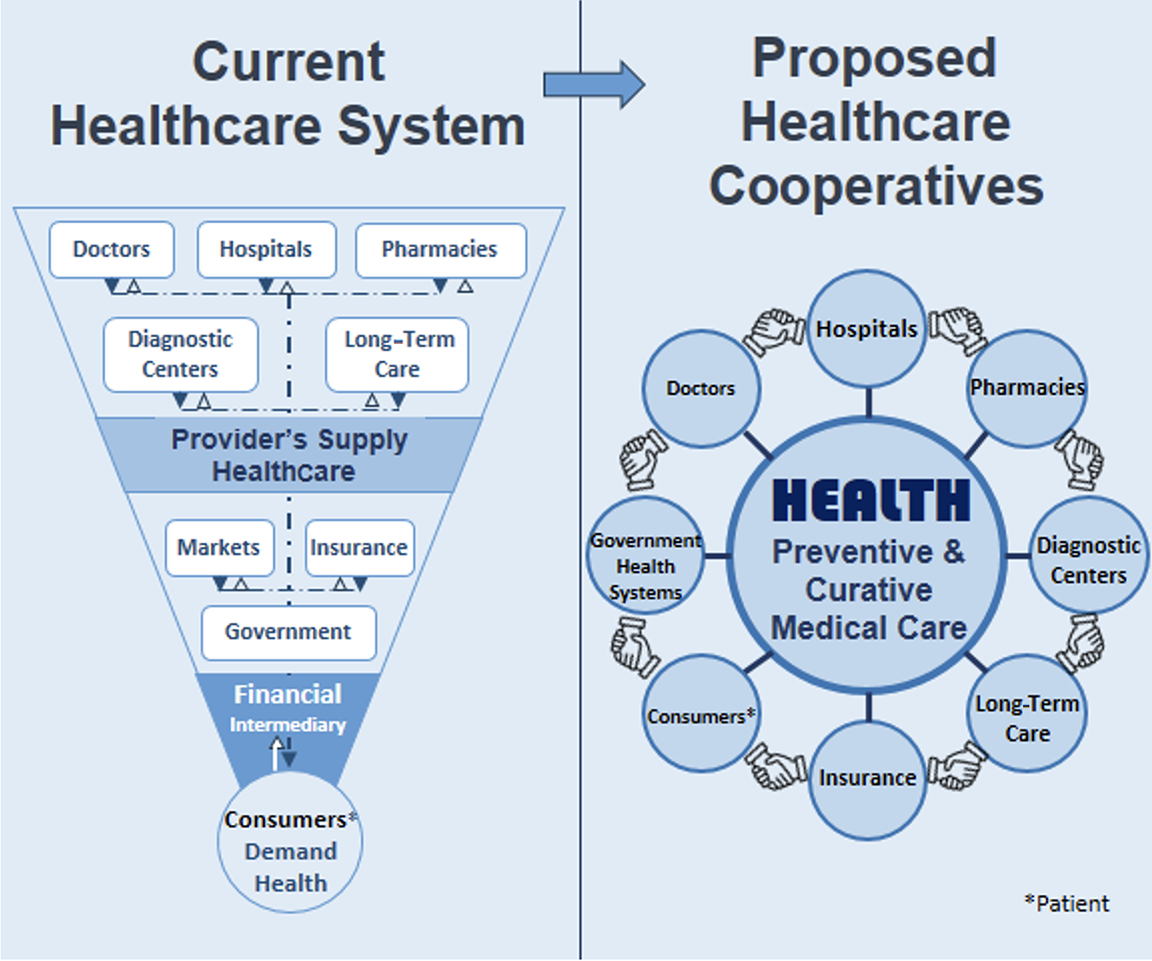
Healthcare systems can be viewed as an organized social response to the health conditions of the population. It is the set of interrelationships between various components of the system that define the characteristics of the system. Components and relationships in the present healthcare system and the proposed one are described in the Figure.
Healthcare providers dispense medical care; however, the population desires health and not medical care alone. Government services are highly centralized, nonparticipatory, and resource-constrained. Insurance providers and markets are profit-oriented. Unfortunately, prevention is better than cure, but preventive services have no markets. In addition, the inputs and outputs of preventive healthcare services are not clearly visible to the stakeholders. The multiple stakeholders in the system with different goals should prioritize population health, and the system should be participatory to preserve the values of human dignity and self-reliance. How can we optimize the system to achieve this?
Figure. A comparison of current and proposed healthcare systems
Proposed multistakeholder healthcare cooperatives
Optimization of the whole healthcare system requires a clear understanding of the goal of the overall system as well as of interactions between the subsystems.
From the financial engineering perspective, the cooperative organization may be a solution to optimize outcomes in this set of diverse portfolios with distributed decision making. Agency theory predicts that agents can behave in bounded rationality and respond altruistically in an appropriate environment.6
Social economy researchers largely predict that such organizations will fail due to the high costs associated with distributed decision making. However, numerous successful examples of multistakeholder cooperatives from Italy and Canada refute this hypothesis.7 The framework that explains the decision-making in these organizations is the one described by Ostrom about collective management of common pool resources.8
Freeman’s stakeholder management model, motivated by a sociogram, asserts that multiple stakeholders can come together to achieve common mutually agreeable goals.9 In this regard, information technology has the potential to link diverse groups on a common platform, allowing each player to get meaningful information about inputs and outputs facilitating effective interaction.
Multistakeholder cooperatives in healthcare delivery can become a reality and pave the way for a novel method of healthcare delivery to achieve universal health coverage and related sustainable development goals. These cooperatives can reconcile the supply and demand of healthcare services by bringing together different stakeholders to jointly manage costs and risks, and to ensure the highest quality of patient-centric care.10
"Healthcare providers dispense medical care; however, the population desires health and not medical care alone."
Examples of healthcare cooperatives across the world
The International Health Cooperative Alliance estimates that there are more than 100 million households worldwide that are served by health cooperatives.11 Examples of health cooperatives in developing countries are in Brazil and Argentina. A significant portion of the healthcare market in Brazil is dominated by cooperatives, with Unimed being both the biggest medical cooperative system in the world and the largest medical care network in the nation.10 In Argentina, cooperatives primarily provide nursing, pharmaceutical, and primary healthcare services. This is because approximately 50% of the population lacks healthcare access due to adverse socioeconomic conditions in the country.10
The history of health cooperatives in India dates back to the 19th century. States like Kerala, Karnataka, and Gujarat have been major players in this domain. The positive impact of healthcare cooperatives can be utilized to reduce the burden on health providers, improve accessibility in remote areas, impart health education and awareness, and provide long-term and home care for terminally ill patients.12
Developed countries also utilize healthcare cooperatives for providing improved healthcare to the population. For example, HealthPartners, United Ag, Mountain Health Co-Op, Group Health in Washington, and Health Partners in Minnesota are large healthcare cooperatives that have flourished in the United States for the past 50 years. They focus on members’ health and well-being and share the profits by providing the best low-cost plans for the members.13 In Spain and Belgium, pharmacy cooperatives have significant market share to provide people with quality and affordable medicines.14
"What is needed is meaningful cooperation of various stakeholders under a systematic framework to achieve a common goal of “Health for All.”
Advantages and disadvantages
Healthcare cooperatives across the world are traditionally where people of similar interests would sell or buy. A major disadvantage of such cooperatives is that one member has one vote for a governing board member by which the system can become a prey to political and other pressures. Multistakeholder cooperatives are a different concept that bring multiple stakeholders in the field of healthcare together in a network of shared investment and profits. The government needs to facilitate the emergence of such cooperatives by advising a regulatory, economical, and legal framework.
The advantages of proposed multistakeholder healthcare cooperatives in India over traditional systems are that they can provide service range expansion (health promotion and prevention to rehabilitation), social care, pharmaceutical range expansion, cost and risk management, quality improvement, adaptability, and sustainability to cover comprehensive preventive care. Staffing, equipping, and managing a healthcare practice is costly. Healthcare cooperatives support that by increasing the average per member recovery versus individuals who pay out of pocket. Improved profitability can also help enhance care quality, leading to better clinical outcomes. Members can proactively take control of their health by establishing good habits.10,13
Conclusion
The application of systems engineering to analyze the healthcare system in India brings forth the solution of multistakeholder cooperatives.
The government of India has already kicked off an initiative, the Ayushman Bharat Cooperative Scheme, in 2020. Although the framework has not yet been widely used, it can serve as a starting point. Two initiatives under National Health Mission (ie, the Patient Welfare Committee and the Village Health, Nutrition, and Sanitation Committee) can help engage various stakeholders together. India is already setting up the system of electronic health records and has a rich pool of talent in information technology. What is needed is meaningful cooperation of various stakeholders under a systematic framework to achieve a common goal of “Health for All.” The balanced provision of preventive care along with curative treatment would go a long way to achieve universal health coverage targets by 2030.15
Acknowledgment: We thank Dr Ashwini Bodas for administrative and technical support and the Maharashtra Medical Research Society (http://mmrs.in) in Pune, India for financial support.
References
- Banatvala N, Bovet P, eds. Noncommunicable Diseases: A Compendium. Routledge; 2023.
- Levine S, Malone E, Lekiachvili A, Briss P. Health care industry insights: Why the use of preventive services is still low. Prev Chronic Dis. 2019;16(180625). doi:10.5888/pcd16.180625
- Gov.in. Accessed May 1, 2024. https://nha.gov.in/PM-JAY
- Nair A, Dubey S, Koshy V, Bansal M, Deshpande S, Zadey S. Solving systemic violence against healthcare workers in India. The BMJ Opinion. Published October 4, 2021. Accessed May 1, 2024. https://blogs.bmj.com/bmj/2021/10/04/solving-systemic-violence-against-healthcare-workers-in-india/
- Declaration of Geneva. World Medical Association. Accessed May 1, 2024. https://www.wma.net/what-we-do/medical-ethics/declaration-of-geneva
- Wolfenden L, Bolsewicz K, Grady A, et al. Optimisation: defining and exploring a concept to enhance the impact of public health initiatives. Health Res Policy Syst. 2019;17(1). doi:10.1186/s12961-019-0502-6
- Lund M, Novkovic S. Multi-stakeholder cooperatives: In Elliot M, Boland M, eds. The Edward Elgar Handbook of Research on Cooperatives and Mutuals. Cheltenham, UK: Edward Elgar publishing (forthcoming). Accessed May 1, 2024. https://rmfu.org/wp-content/uploads/Multi-Stakeholder-Cooperatives-MSCs_Novkovic_Lund_2023_Final-version.pdf
- Šestáková A, Plichtová J. Contemporary commons: sharing and managing common-pool resources in the 21st century. Hum Affairs (Tlacene Vyd). 2019;29(1):74-86. doi:10.1515/humaff-2019-0007
- Tam M. Stakeholder theory: Edward Freeman. Stakeholdermap.com. Published October 15, 2015. Accessed May 1, 2024. https://www.stakeholdermap.com/stakeholder-theory-freeman.html
- Healthcare cooperatives: a reliable enterprise model for health and wellbeing. United Nations. Accessed May 1, 2024. https://www.un.org/development/desa/cooperatives/wp-content/uploads/sites/25/2019/03/190326_ihco_EGM-nairobi.pdf
- International Cooperative Alliance. In: Handbook of Transnational Economic Governance Regimes. Brill | Nijhoff; 2010:155-167.
- Devasoorya RM, Srinivasa Vallabhan SV. Healthcare co-operatives: possible third realm of healthcare in India. Published online October 28, 2016. doi:10.2139/ssrn.2860548
- Healthcare Co-Ops. NCBA CLUSA. Published June 4, 2019. Accessed May 1, 2024. https://ncbaclusa.coop/resources/co-op-sectors/healthcare-co-ops/
- Spain: Pharmaceuticals. World Health Systems Facts. Published December 22, 2020. Accessed July 21, 2024. https://healthsystemsfacts.org/spain/spain-pharmaceuticals
- Ayushman Sahakar. A scheme of NCDC for financial assistance to cooperatives on holistic healthcare infrastructure, education and services. National Cooperative Development Corporation. Ministry of Agriculture and Farmers Welfare. New Delhi 2020. https://www.ncdc.in/documents/downloads/03171603234509191020AS-Eng-Full.pdf

