Are We Leaving No One Behind? Health Technology Assessment as a Pathway to Social Justice
Lucia Perez Kempner, MSc, MBS, Parexel International, Sevilla, Spain; Chiamaka Akunne, BS, Parexel International, Burlington, NJ, USA
Health equality and/or equity as a path to development
While the right to good health is considered a basic human right, many populations suffer from poor health. Globally, cross-group comparisons suggest health inequalities, which imply unequal distributions of health states across populations.1-3 Evidence indicates high prevalence of health inequities, which occur when health inequalities are the result of unjust, systematic, and avoidable factors related to the social determinants of health (SDH).4 Health inequities between groups may stem from differences in demographics, socioeconomic status, educational status, healthcare access, environmental exposure, etc. The promotion of health equality and equity has been recognized by global institutions, such as the World Health Organization and the United Nations, as a means to address unfair differences in health across populations.4 Specially, the United Nations’ Sustainable Development Goals highlight improving access to quality healthcare and essential medicines across populations as a key objective to ensuring health equality and equity.5
The use of health technology assessment (HTA) has been identified by global institutions as a potential means to advancing health equality and equity. While HTA reviews have been intended historically to ensure an optimal use of finite healthcare resources, there is a growing recognition that HTA can also reduce health disparities across populations.6 However, the extent to which HTA agencies actively consider health equality and/or equity promotion as a component of their assessments is relatively uncharacterized, increasing the need for research into this area.
Evaluation of health equality and/or equity considerations in HTA policies
The objective of this research was to identify HTA appraisal frameworks in high- and middle-income countries (HICs, MICs) to assess whether considerations of health equality and/or equity are included as core principles of the HTA decision-making process. To accomplish this objective, we selected Europe as a region in which most HICs have established HTA entities, and Latin America and Asia as regions in which HICs and MICs are in the process of establishing HTA entities. We identified a total of 20 countries with established formal HTA entities: 5 each in Western Europe, Northern Europe, Latin America, and Asia. We reviewed the HTA appraisal frameworks from each country and identified those in which health equality and/or equity were considered as part of the decision-making criteria. We also reviewed initiatives by the Centers for Medicare & Medicaid Services (CMS) and the Institute for Clinical and Economic Review (ICER) in the United States. CMS, the public insurer for the aged and disabled population, is a critical player given its high purchasing and influencing power across all insurers in the United States. Moreover, ICER is also a critical player given its increasing influence over CMS and international collaboration on HTA processes.
Global efforts to advance towards health equality and/or equity goals
Equality and/or equity as criteria for HTA decision making
We identified the appraisal frameworks of formal HTA agencies in Argentina, Brazil, Chile, China, Colombia, England, Finland, France, Germany, Iceland, Italy, Kazakhstan, Malaysia, The Netherlands, Norway, Peru, South Korea, Spain, Sweden, and Taiwan (Table 1). Among these, we identified 8 countries (Argentina, Chile, China, England, Finland, Norway, The Netherlands, and Sweden) in which HTA appraisal frameworks include health equality and/or equity within the criteria used to evaluate health technologies. The health equality and/or equity principle is mostly used to guide decision making on the prioritization of health technologies to be evaluated by HTA agencies from the pool of available technologies awaiting evaluation. In a few instances, the principle is also used to guide decision making during the technical appraisal of the health technology under evaluation.
Table 1. Use of health equality and/or equity principles for HTA decision making
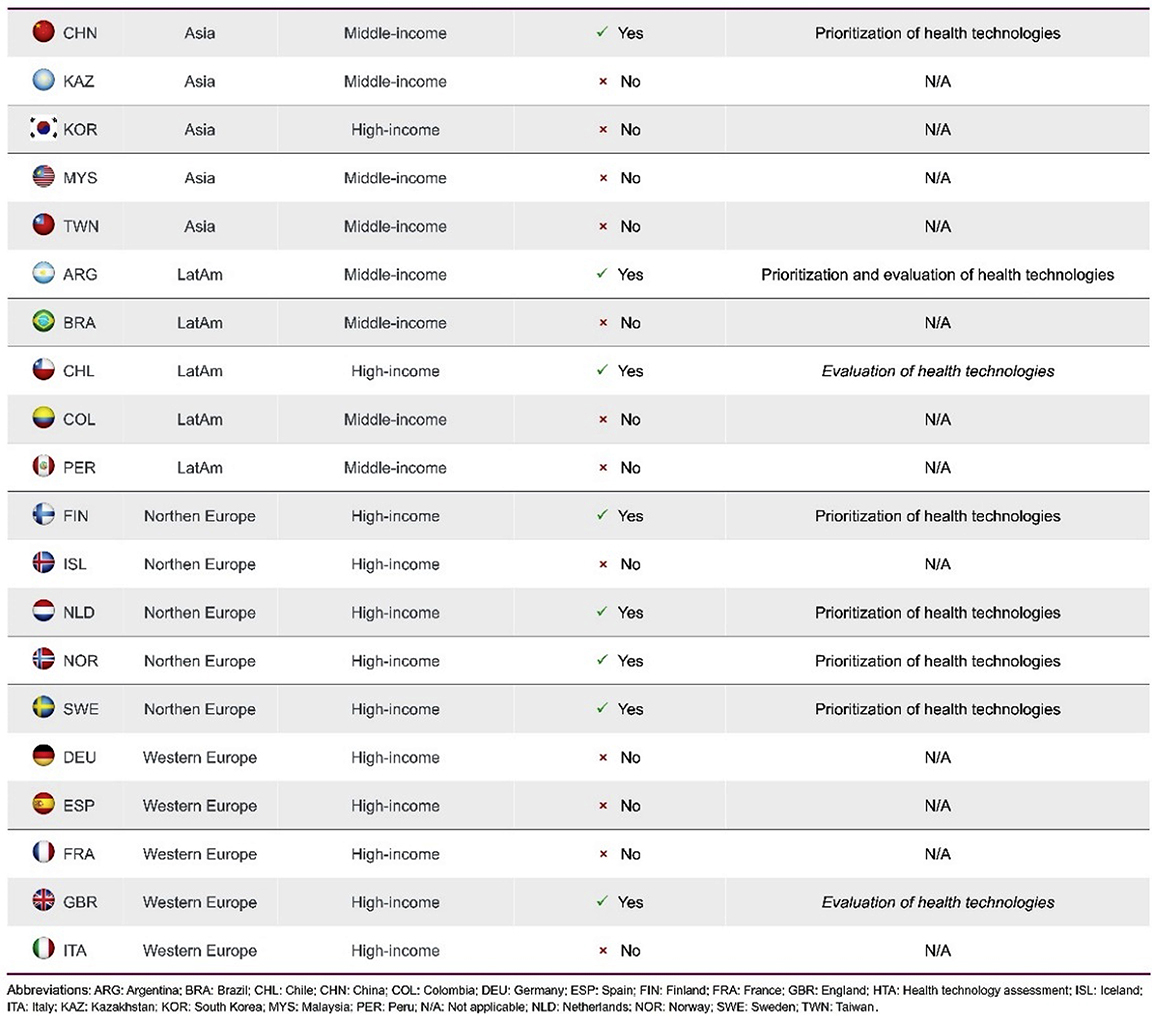
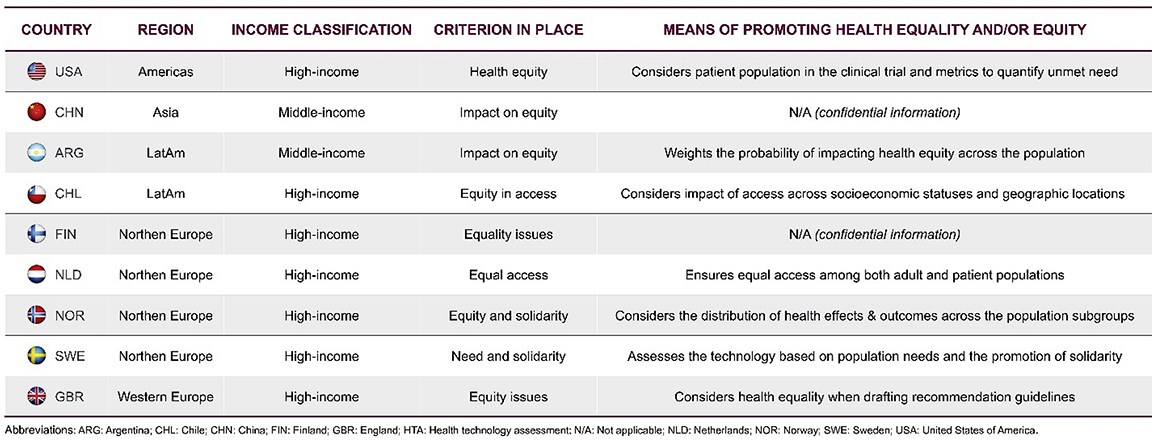
Furthermore, we observed that the criteria in place used to incorporate health equality and/or equity in the decision-making process and the means for promoting health equality and/or equity were subjective, broadly defined, lacked specific metrics for quantification, and varied greatly across countries (Table 2). Among the criteria in place, equity was explicitly mentioned in Argentina, Chile, China, England, and Norway, emphasizing the commitments by these countries to not only improve health outcomes but also reduce social injustice and provide the resources needed for disadvantaged populations. In particular, in Chile, the decision-making policy directly linked the equity criterion to the determinants of health. In China and Finland, the means of promoting health equality and/or equity were confidential and not publicly disclosed.
In the United States, as there is no national HTA process or agency, we identified the appraisal framework and decision-making initiatives of ICER. We found that ICER has announced the Value Assessment Framework (VAF) initiative to evaluate changes in its methodology for the assessment of technologies in order to advance health equity goals. The initiative involves the evaluation of potential changes to the current methodology by an advisory board, followed by updates to the VAF in the future. In 2023, ICER announced that the VAF will focus on 2 HTA methods related to health equity: analyses of clinical trial diversity and racial/ethnic subpopulations and quantitative measures to guide discussion and voting on unmet need (Table 2).
Table 2. Health equality and/or equity principles in place and means of promoting health equity and/or equity across HTA decision-making
"Health equality and/or equity principles within HTA appraisal frameworks remain broad, subjective, and unquantifiable, calling for objective data analysis to quantify health equality and/or equity."
Governmental efforts to advance health equity in the United States
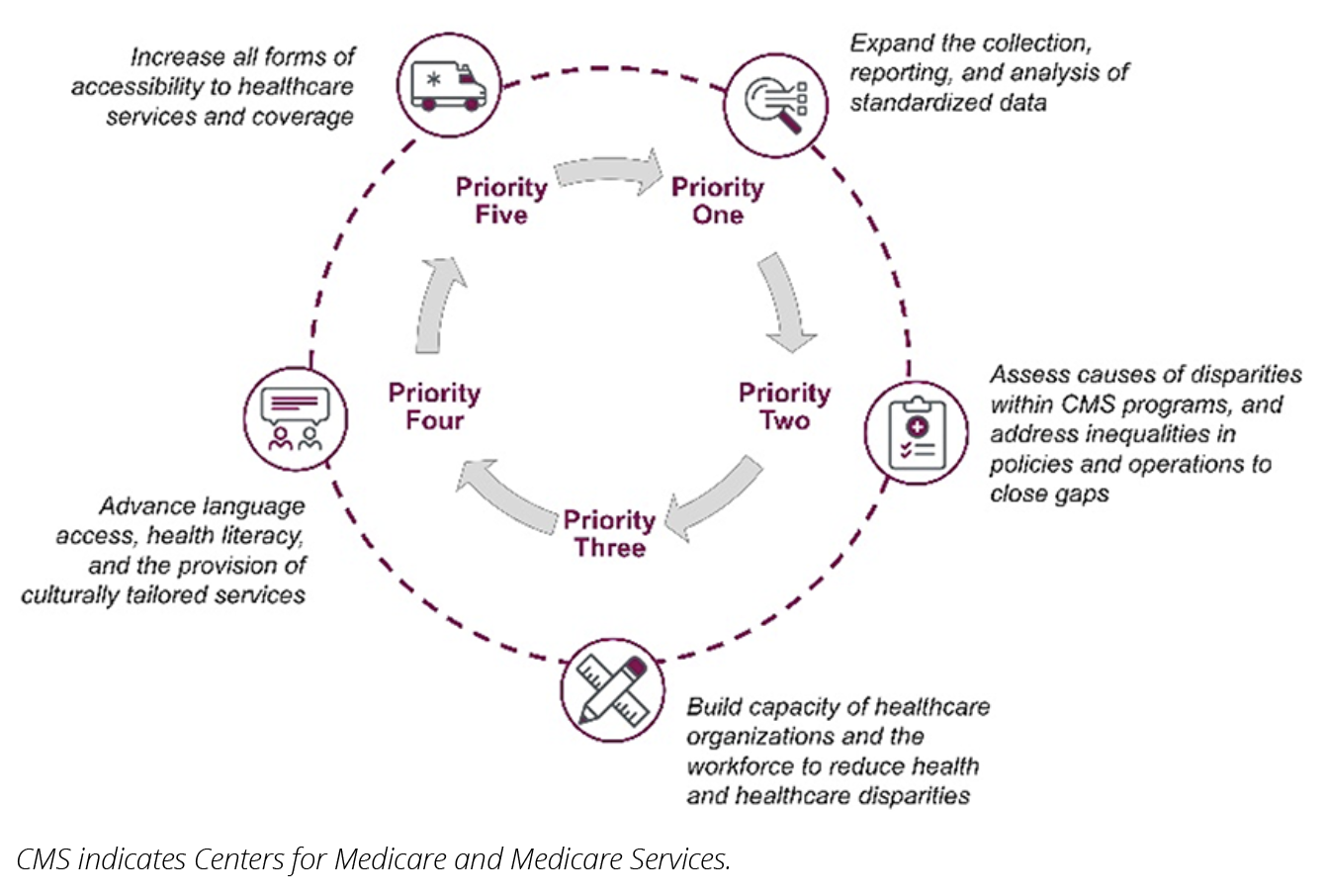
Given the lack of national HTA process or agency in the United States, we also identified efforts by CMS to enable the inclusion of value in its decision-making process and promote equity, including the agency’s “Framework for Health Equity 2022-2032”.7,8 The framework aims to promote health equity, increase healthcare access, and improve health outcomes among CMS beneficiaries. The program is based on 5 priorities that include assessing existing health disparities and developing solutions to address them (eg, increasing access to healthcare services and coverage) (Figure 1). The framework focuses on data collection and analysis to support evidence-based decision making, resource and capacity building to improve equal access to infrastructure and equipment, and patient support and empowerment of populations.
Figure 1. CMS framework for health equity priorities
Moreover, CMS has also implemented performance-based payment programs to improve health equity. The Enhancing Oncology Model is a 5-year program intended to improve the quality of healthcare, while decreasing the associated costs and reducing health disparities related to SDH.9 To accomplish these goals, the program implements payment incentives and disincentives for participating clinicians, which include monthly enhanced oncology services payments, performance-based payments, and performance-based recoupments. This is in line with existing payment policies that CMS is implementing to address SDH. Participants are required to develop health equity plans that address SDH in order to reduce health disparities among beneficiaries.9,10
Another CMS program is the ACO REACH model (Accountable Care Organization Realizing Equity, Access, and Community Health).11 This model was developed to test innovative payment approaches to better support the delivery of care and patient coordination in underserved communities. Participants are required to identify underserved communities and implement initiatives to reduce health disparities among beneficiaries of the model.
The way forward—strengthening health systems and value communication
This research shows that efforts to advance health equality and/or equity, which have been on the global health agenda for the past 25 years, are now being incorporated into national decision-making processes. With HICs leading the movement, countries are moving towards evidence- and equality- and/or equity-based decision-making frameworks that consider the impact of SDH on access to new health technologies and the impact that these technologies may have on efforts to advance health equality and/or equity. As countries with established HTA agencies refine their HTA processes, and countries with emerging HTA agencies define their HTA processes, there is room for improvement towards equality- and/or equity-based decision making.
Nonetheless, health equality- and/or equity-based criteria for HTA decision making remains broad, subjective, and/or undefined in the appraisal framework of several HTA agencies selected in this research. This lessens the impact of the criteria on the final HTA decision-making process. It is imperative that HTA agencies should consider incorporating equity considerations into frameworks for assessing cost-effectiveness by mandating the use of analytical methods that consider equity within a health system (eg, distributional cost-effectiveness analysis). HTA bodies should also define and implement analytical parameters, such as the Health Equity Index, to objectively quantify health equality and/or equity at baseline and the impact that new health technologies will have on the health equality and/or equity of the population. HTA agencies must also develop frameworks to help manufacturers address data gaps (eg, in clinical trial data and in economic evaluations) that may limit the ability to make this quantification. Global collaboration among HTA agencies, academics, and policy makers could help advance these efforts. Nonetheless, practical challenges for the implementation of the above-mentioned strategies, driven by differences in patient populations and health system structures, will need to be overcome.
"Efforts to advance health equality and/or equity, which have been on the global health agenda for the past 25 years, are now being incorporated into national decision-making processes."
As national efforts to support health equality and/or equity advance, it is imperative that HTA agencies consider policies that request manufacturers to consider health equality and/or equity in their HTA submissions. Such policies may drive manufacturers to consider the impact that their new health technologies would have on health equality and/or equity in the healthcare systems of each country or region, and the data required to demonstrate it. This impact should become a component of value-added services that can target SDH to reduce health inequality and/or inequity, and of the value proposition of new health technologies, in line with value propositions on disease burden, unmet need, and clinical, humanistic, and economic value. This value proposition on health equality and/or equity should be incorporated into the value story, value communication, and overall value strategy of new health technologies throughout their life cycles. Furthermore, the quantification of economic gains to health systems resulting from reduced health inequalities and/or inequities due to access to the new health technologies could provide additional support to innovative payment methods seeking to advance health equality and/or equity and to economic value claims that present the direct and indirect benefits of the new health technologies. This would be the most critical in countries that follow a societal perspective for their HTA decision making, such as Sweden and other countries in the North-European region.
References
- Lee J, Phillips D, Wilkens J, et al. Cross-country comparisons of disability and morbidity: evidence from the gateway to global aging data. J Gerontol A Biol Sci Med Sci. 2018;73(11):1519-1524.
- GBD 2019 Diseases and injuries collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222.
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249.
- Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015;8:27106.
- United Nations Development Programme. What are the Sustainable Development Goals? 2024. Accessed March 1, 2024. https://www.undp.org/sustainable-development-goals
- Institute for Clinical and Economic Review (ICER). Advancing Health Technology Assessment Methods That Support Health Equity. 2023. Accessed March 1, 2024. https://icer.org/wp-content/uploads/2022/07/ICER_Advancing-Health-Technology-Assessment-Methods-that-Support-Health-Equity_03152023.pdf
- Centers for Medicare & Medicaid Services (CMS). CMS Framework for Health Equity 2022–2032. 2022. Accessed March 1, 2024. https://www.cms.gov/files/document/cms-framework-health-equity-2022.pdf
- Centers for Medicare & Medicaid Services (CMS). CMS Framework for Health Equity. 2023. Accessed March 1, 2024. https://www.cms.gov/priorities/health-equity/minority-health/equity-programs/framework
- Centers for Medicare & Medicaid Services (CMS). Enhancing Oncology Model. 2024. Accessed March 1, 2024. https://www.cms.gov/priorities/innovation/innovation-models/enhancing-oncology-model
- Centers for Medicare & Medicaid Services (CMS). Enhancing Oncology Model (EOM): Health Equity Strategy. Accessed March 1, 2024. https://www.cms.gov/priorities/innovation/media/document/eom-healthequity-fs
- Centers for Medicare & Medicaid Services (CMS). ACO REACH. 2024. Accessed March 1, 2024. https://www.cms.gov/priorities/innovation/innovation-models/aco-reach

