Application of Real-World Data Sources for Equity-Informative Evaluations in the United States: A Multiple Myeloma Case Study
Salome Ricci, PharmD, MS, Eberechukwu Onukwugha, PhD, MS, Jean Yared, MD, and Julia Slejko, PhD, University of Maryland, Baltimore, MD, USA
Introduction
Incorporating health equity into value and health technology assessment (V/HTA) is a major focus in health economics and outcomes research, as evidenced by a previous Value & Outcomes Spotlight theme (May/June 2024), Value in Health papers, and an active ISPOR Health Equity Special Interest Group.1 Publications from the European Society of Medicine and the Center for Innovation & Value Research emphasize the importance of integrating health equity into healthcare evaluations.2,3 A common theme is the need for data generation to inform high-quality evaluations on equity-relevant topics. In this article, we examine this topic from a US perspective using multiple myeloma (MM) as a case study and expand on research presented at ISPOR Europe 2023.4
MM is a hematologic malignancy characterized by abnormal proliferation of monoclonal plasma cells in the bone marrow. It predominantly affects older adults, with a median age at diagnosis of 69 years. In 2024, 35,780 new cases were diagnosed in the United States, with a 5-year relative survival rate of about 61%.5 Although novel therapies have greatly improved outcomes, MM remains incurable, and patients often experience multiple relapses and die from their disease.6
Health disparities in MM
Disparities in MM outcomes result from a complex interplay of factors. Evidence suggests differences in disease biology between racial and ethnic groups, such as variations in cytogenetics and molecular alterations that could affect prognosis, treatment decisions, and outcomes. The incidence of MM is at least twice as high in Black individuals compared to White individuals, and lowest among Asians and Pacific Islanders.6
Despite a higher disease incidence, Black individuals are underrepresented in clinical trials, comprising about 6% of US participants but approximately 20% of US cases.7 Real-world studies show disparities extend beyond the clinical trials setting, with discrepancies in access to triplet induction treatment, autologous stem cell transplantation (ASCT), and CAR-T cell therapy for these groups. For instance, one study found Black and Hispanic individuals experienced longer times from MM diagnosis to novel therapy initiation compared to White individuals, with median times of 5.2 and 4.6 months versus 2.7 months, respectively.8 Sociodemographic disparities further exacerbate inequities, affecting access to diagnostic testing, timely treatment, and novel therapies. Socioeconomic factors such as lower income and lack of insurance coverage can negatively influence the likelihood of receiving timely MM diagnosis and treatment, consequently worsening outcomes. For example, a study found that low socioeconomic status was associated with poorer overall survival, showing a 54% increase in mortality compared to those with higher socioeconomic status.9
Disparities in treatment and survival among individuals diagnosed with MM are driven by systemic factors and social determinants of health, along with genetic differences, cultural beliefs, medical mistrust, and variations in disease management. Overcoming these disparities requires a multifaceted approach that considers both systemic and individual factors to promote equity among individuals diagnosed with MM.
"Evidence suggests differences in disease biology between racial and ethnic groups, such as variations in cytogenetics and molecular alterations that could affect prognosis, treatment decisions, and outcomes."Leveraging real-world data
Real-world data (RWD) offer a valuable resource for understanding how MM affects various populations and supporting equity-informative evaluations of MM therapies. By leveraging RWD, researchers can better assess the extent of health inequities and their impact on disease progression and treatment outcomes.
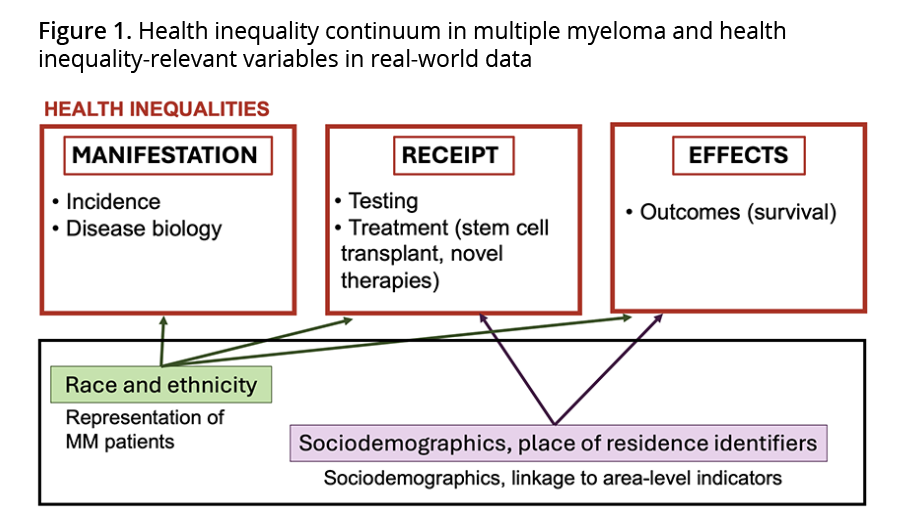
We conceptualized how health inequality-relevant variables influence disease manifestation, access, and outcomes of patients with MM. [Figure 1] Race and ethnicity are key factors, as they differentially affect the need for care due to differences in incidence and disease biology, which can impact treatment decisions and access. Sociodemographic factors play a significant role as well. Marital status may indicate the presence of a caregiver and may be associated with the likelihood of receiving an ASCT, leading to differences in outcomes. Socioeconomic factors such as income are essential in determining access to timely diagnosis and treatment options, influencing survival rates and quality of care. When sociodemographic and socioeconomic data are not readily available, residential data can provide valuable contextual information. Area-level variables such as county-level median income can offer important insights into the role of the individual’s socioeconomic environment when these variables are linked to RWD that include the patient’s ZIP code or county of residence. In fact, our prior work found significant associations between county-level indicators of deprivation and both MM treatment type and subsequent outcomes.10
Multiple data sources fill the gaps
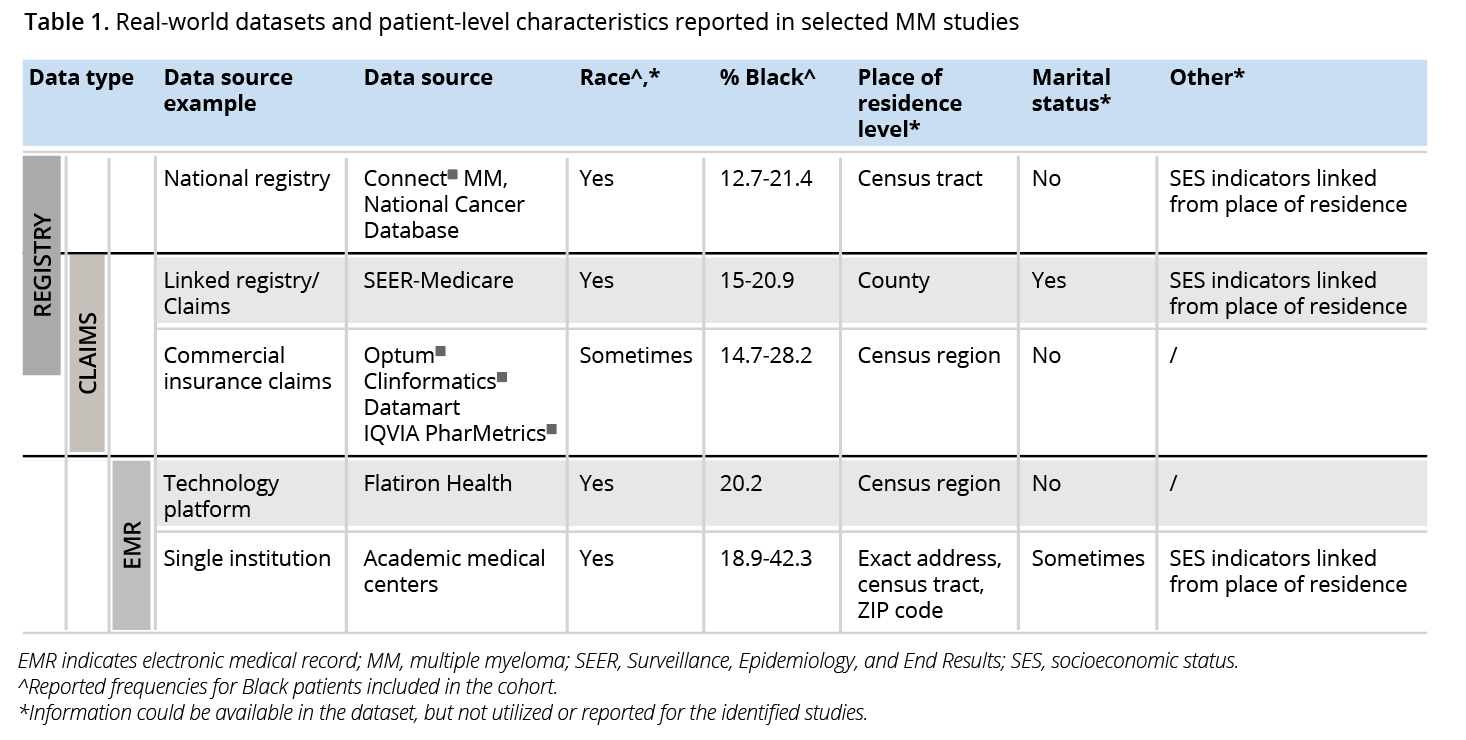
A key question is whether RWD can fill in the evidence gaps that remain owing to underrepresentation of racial and ethnic groups in MM clinical trials. We reviewed the literature to identify datasets that have been cited in past RWD studies of MM outcomes. Datasets were organized into categories based on key characteristics. We identified and reported patient characteristics that can be employed in MM equity-informative studies. We focused on whether race was reported in these studies, and if so, the proportion of Black patients.
Our findings illustrate the variability in RWD sources. [Table 1] Real-world databases like Optum’s Clinformatics® Data Mart and the Surveillance, Epidemiology, and End Results (SEER) data linked to Medicare claims, cover large populations, making them valuable for understanding healthcare utilization patterns and economic aspects of care. However, these data sources often lack detailed clinical and demographic information, such as race and ethnicity or place of residence. When available, Black patient representation ranged from 14.7% to 28.2%, demonstrating a considerable degree of diversity. Survival outcomes may also be limited in claims data, restricting their use in longitudinal studies.
"By leveraging RWD, researchers can better assess the extent of health inequities and their impact on disease progression and treatment outcomes."
Electronic health records data offer rich clinical details, including laboratory results, treatment responses, and patient histories. They often include sociodemographic information such as race, marital status, and place of residence, allowing for more nuanced analyses of health disparities. However, they are confined to encounters within specific healthcare systems, which may not capture all the care an individual receives. This confinement can also limit their sample size and generalizability. Nevertheless, the clinical and sociodemographic information provided is extremely rich. These data sources can exhibit high representation of Black patients, with single institution data showing such proportions up to 42.3%, the highest among the data sources examined.
Integrating multiple data sources can significantly enrich research findings by combining the strengths of each data type while mitigating their limitations. However, merging data from different sources requires careful consideration of data compatibility and privacy concerns, as well as addressing technological hurdles. Ensuring accurate linkage and maintaining patient confidentiality are critical.
Path to equity: engaging stakeholders
Understanding and addressing disparities requires a coordinated effort from all stakeholders—patients, healthcare providers, policy makers, and pharmaceutical companies—to achieve equity and ensure that all patients receive effective and timely interventions. For healthcare providers, recognizing the disparities in MM is essential for delivering equitable care. Providers can better address diverse patient needs by fostering trust, open communication, and cultural sensitivity and engaging with MM patient communities. Additionally, growing evidence about the impact of disparities in access and outcomes can inform and inspire action. Highlighting successful outcomes of patients with MM across communities who receive high-quality care can encourage best practices and drive improvements in care delivery. The patient’s experience with MM care could be influenced by the treatment setting—whether a community practice or academic center—and the characteristics of the treating physician (eg, years of experience, clinical practice setting). Differences in treatment decisions, access to advanced therapies, adherence to guidelines, and facility type can lead to varying patient outcomes. RWD, particularly individual patient data linked to healthcare-, provider-, and hospital-level characteristics, provide an opportunity to study provider-level variations, identify patterns that contribute to disparities, and better understand the relationship between patient demographics, provider behaviors, and care settings.
Policy makers can leverage findings from RWD studies to inform policies that address healthcare inequities, such as promoting diversity in clinical trials and equitable resource distribution. However, using RWD for health technology assessment (HTA) is challenging due to the limited data availability at the time new treatments are assessed. Proactive approaches, including preplanned data collection and the use of modeling techniques, can support equity impact analysis before substantial RWD are available. Combining quantitative RWD with qualitative insights from patient communities can help embed health equity considerations into HTA processes. This aligns with recent calls for standardized health equity frameworks and metrics, allowing assessments to evolve as more data become available.1-3
"For pharmaceutical companies, a priority is to understand outcomes across groups who experience access barriers, such as the uninsured or those needing help navigating the healthcare system."
For pharmaceutical companies, a priority is to understand outcomes across groups who experience access barriers, such as the uninsured or those needing help navigating the healthcare system. Mixed methods can be used to understand unmeasured factors and guide improvements to ensure all patient populations benefit from new treatments. These insights can also inform initiatives aimed at increasing representation in clinical trials, such as targeted recruitment efforts and partnerships with community organizations.
Conclusion
The necessity of robust data generation to support high-quality evaluations is a recurring theme across efforts to incorporate health equity considerations into value and health technology assessment. Using MM as a case study in the United States, we illustrate how RWD can serve as an important resource to support equity-informative evaluations and to fill in evidence gaps from clinical trials. Through data-driven approaches, the healthcare community can strive towards increasing equity in value assessments and access to treatment.
References
- Health Equity. Value & Outcomes Spotlight. 2023;10(2).
- Innovation and Value Initiative. No Value Without Equity: Transforming Practice and Accountability for Equity in Health Technology Assessment. March 2023. Accessed September 12, 2024. https://valueresearch.org/wp-content/uploads/2024/01/No-Value-Without-Equity_Synthesis-Insight.pdf
- Garfield S, Armstrong S, Nguyen J, et al. Are health technology assessments keeping pace with health equity priorities: a review of existing approaches and discussion of emerging practices. Med Res Arch. 2023;11(6). https://doi.org/10.18103/mra.v11i6.3903
- Ricci S, Pernati CV, Onukwugha E, Yared JA, Trovato JA, Slejko JF. RWD51 Application of real-world data sources for equity-informed evaluations of multiple myeloma. Value Health. 2023;26(12):S513–S514. https://doi.org/10.1016/j.jval.2023.09.2768
- American Cancer Society. Key statistics about multiple myeloma. Accessed April 11, 2024. https://www.cancer.org/cancer/types/multiple-myeloma/about/key-statistics.html
- Blue B, Pierre A, Mikhael J. Culturally responsive care delivery in oncology: the example of multiple myeloma. Clin Lymphoma Myeloma Leuk. 2023;23(9)651-659. https://doi.org/10.1016/j.clml.2023.05.005
- Kanapuru B, Fernandes LL, Fashoyin-Aje LA, et al. Analysis of racial and ethnic disparities in multiple myeloma US FDA drug approval trials. Blood Adv. 2022;6(6):1684–1691. https://doi.org/10.1182/bloodadvances.2021005482
- Ailawadhi S, Parikh K, Abouzaid S, et al. Racial disparities in treatment patterns and outcomes among patients with multiple myeloma: a SEER-Medicare analysis. Blood Adv. 2019;3(20):2986–2994. https://doi.org/10.1182/bloodadvances.2019000308
- Fiala MA, Finney JD, Liu J, et al. Socioeconomic status is independently associated with overall survival in patients with multiple myeloma. Leuk & Lymphoma. 2015;56(9):2643–2649. https://doi.org/10.3109/10428194.2015.1011156
- Hong YD, Mullins CD, Onukwugha E, Yared JA, Zheng Z, Slejko JF. Association of individual low-income status and area deprivation with mortality in multiple myeloma. J Geriatr Oncol. 2023;14(2):101415. https://doi.org/10.1016/j.jgo.2022.12.003

