Health Economic Modeling in Obesity: Does the Structure Matter?
Bjoern Schwander, PhD, AHEAD GmbH - Agency for Health Economic Assessment and Dissemination, Bietigheim-Bissingen, Germany; Mark Nuijten, PhD, a2m - Ars Accessus Medica, Amsterdam, The Netherlands; Silvia Evers, PhD, CAPHRI - Care and Public Health Research Institute, Maastricht University, Maastricht, The Netherlands; Mickaël Hiligsmann, PhD, CAPHRI - Care and Public Health Research Institute, Maastricht University, Maastricht, The Netherlands
Background and Introduction
This research presents the lessons learned from a 5-year research project at Maastricht University aiming to increase trust and confidence in selecting and interpreting results related to commonly applied structural approaches used in health economic obesity models.1
Obesity is an abnormal or excessive fat accumulation often defined as a body mass index >30 kg/m2 (BMI).2 Obesity reached epidemic proportions and is a leading risk for global deaths and morbidities.3 Worldwide, obesity among adults has more than doubled since 1990. The global age-standardized prevalence of obesity increased from 8.8% in 1990 to 18.5% in 2022 in women and from 4.8% to 14.0% in men.4
Accordingly, global healthcare systems are facing populations with increasing prevalences of obesity-associated diseases, such as type 2 diabetes, coronary heart disease, stroke, osteoarthritis, different cancer types, and others. Besides the severe health consequences of these diseases, the World Obesity Federation predicted that the global economic impact of overweight and obesity will reach $4.32 trillion annually by 2035, if prevention and treatment measures do not improve.5
"Obesity reached epidemic proportions and is a leading risk for global deaths and morbidities."
To evaluate the impact of such prevention and treatment measures on the chronic obesity-associated diseases and the related burden to patients and healthcare payers, health economic (HE) models are frequently applied. The results of such HE models are centrally triggered by the chronic nature of the obesity-associated diseases that develop over a long time horizon. In a perfect world, long-term clinical studies would be performed to evaluate the impact of obesity prevention and treatment measures on chronic obesity-associated diseases. Because time and funds are limited, and decisions on the best available strategies are required to be made as soon as possible, clinical studies often focus on short-term surrogate parameters. Such surrogate parameters are, for example, the weight or BMI development, but also the development of known risk factors (eg, blood pressure, cholesterol values, etc) for obesity-associated diseases. Thus, to determine the value of an intervention, these short-term surrogates need to be translated into obesity-associated diseases to predict the associated quality of life and cost consequences adequately.
Our research, summarized in this paper, focused on the systematic evaluation, replication, and validation of modeling approaches in the context of obesity. A special emphasis was set on the methodology to translate (short-term) surrogate parameters into (long-term) obesity-associated diseases, which represents a central structural decision to be made when developing a HE obesity model.
A stepwise process was followed. First a systematic review was performed to determine which clinical events were commonly simulated in obesity models and how these clinical events were simulated. Hence, all HE models that simulated obesity-associated diseases were included, irrespective of whether events were simulated as acute or chronic health states/conditions or discrete events. The approaches applied to simulate such obesity-associated diseases are named event simulation approaches throughout this manuscript. Second, a replication of high-quality HE obesity models, reflecting the main event simulation approaches, was performed and the reproduction success was evaluated. Finally, using the successfully replicated models, an external validation was performed using state of the art methods applied in comparable research.6,7 To assess external validation, predicted outcomes were plotted against empirical study endpoints to visually inspect concordance, quantified using linear regression analysis (slope and intercept), categorized deviation from optimal slope (±25%, ±50%, ±100%), and further evaluated using R2, F test for line identity, and root mean square error (RMSE) for model fit accuracy. Furthermore, the influence of the structural event modeling approach on the HE modeling results was investigated, focusing on the central result parameter of HE assessments, the incremental cost-effectiveness ratio (ICER).
"In a perfect world, long-term clinical studies would be performed to evaluate the impact of obesity prevention and treatment measures on chronic obesity-associated diseases."
Results
As a result of the systemic literature search, 87 papers reflecting HE obesity models were identified. It was found that most research teams built their own HE model (79%) and that only a minority used a previously published model (21%). Only for a minority (14%) of the model-based HE assessments in obesity was an external event validation was performed.
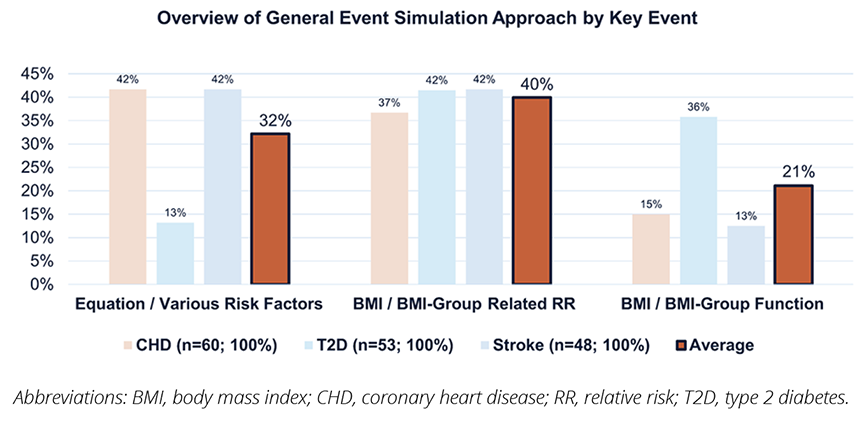
Most frequently simulated clinical events were coronary heart disease (≈83%), type 2 diabetes (≈74%), and stroke (≈66%). These 3 obesity-associated key events were simulated by 39 models (≈54%). As presented in Figure 1, we categorized the obesity-associated event simulation approaches into 3 major methodologies, identified as: 1) Equation/various risk factors: established risk functions/equations (eg, Framingham8,9 or UKPDS10) were used to estimate the risk of an event or condition; in these cases the intervention effect was estimated by simulating the intervention’s impact on the risk equation’s risk factors (such as systolic blood pressure, age, diabetes status, etc); 2) BMI/BMI group–related relative risk: the base risk of the events was estimated using different incidence estimation approaches (potential impact fraction, age, gender, etc) and a BMI or BMI group–specific relative risk (RR) was applied in order to estimate the intervention effect on the frequency of obesity-associated events; 3) BMI/BMI group function: the base risk was estimated on the basis of the BMI or a BMI group (BMI is the central part of the risk equation applied); hence, the intervention effects on the BMI or he BMI group directly impacted the base risk.
Figure 1. Methodological Variations—Event Simulation Approaches in Obesity Models
In a next step, 4 high-quality HE obesity models11-14 were selected and a model replication was performed using TreeAge Pro. The model selection process (based on the outcomes of an expert panel consensus15) involved satisfying criteria for long-term simulation, specific model types (state transition or discrete event simulation), key simulated events (coronary heart disease, type 2 diabetes, stroke), and applicability to the UK adult population.
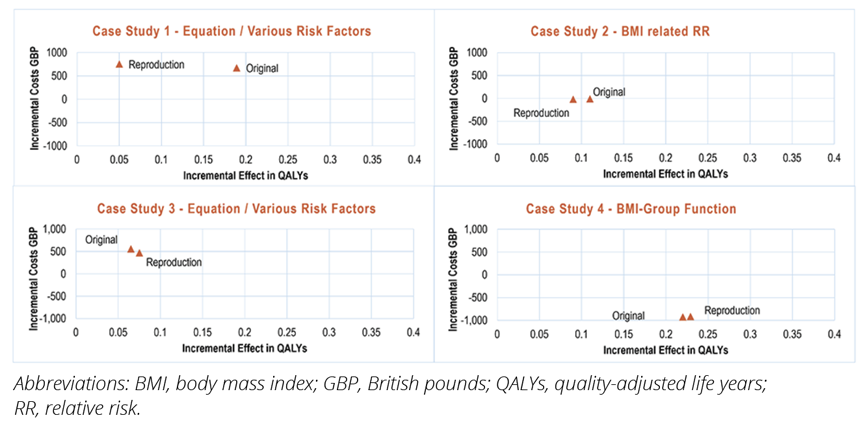
All 4 case studies were state-transition models simulating costs and quality-adjusted life years (QALYs). The reproduction success for model results was measured with several factors.16 The applied criteria for measuring replication success involved a combination of standards, focusing on achieving identical cost-effectiveness conclusions, ensuring acceptable deviations in individual components (<5%), and obtaining comparable ICERs. As shown in Figure 2, incremental costs and incremental QALY visualized on a plane were the key factors for evaluating the combined reproduction success. Accordingly, case study 1 was rated as a failure, due to the visualized huge deviation of original and replicated incremental QALY results, and case studies 2, 3, and 4 as successes in reproducing results.
Figure 2. Model Result Reproduction Success—Variations of Incremental Costs and Effects by Case Study
Using the 3 successfully replicated models, an external validation using the Swedish obesity subjects (SOS) study17 was performed. The SOS study compares long-term health outcomes between individuals who undergo bariatric surgery and those receiving conventional obesity treatments. It was selected as a validation study as it is currently the only available prospective long-term intervention study in obese subjects that has presented statistically significant improvements in mortality, incidence of type 2 diabetes, and fatal/nonfatal cardiovascular events (myocardial infarction and stroke) for obesity surgery compared to matched controls over an 18-year period.
These replicated models reflect 3 main structural event-modeling approaches used in obesity outlined above: 1) Equation/various risk factors; 2) BMI-related RR; and 3) BMI group function. Concordance between modeling results and the SOS study were investigated by linear regression analyses and different measurements (outlined in the methods), and then they were categorized by the grade of deviation observed (from grade 1–4 expressing mild, moderate, severe, and very severe deviations), as presented in Figure 3. Overall and by study arm, the risk equation approach showed a better overall event prediction than the BMI-related RR approach, followed by the BMI group function.
Figure 3. External Validation Results—Grade of Deviation by Key Event
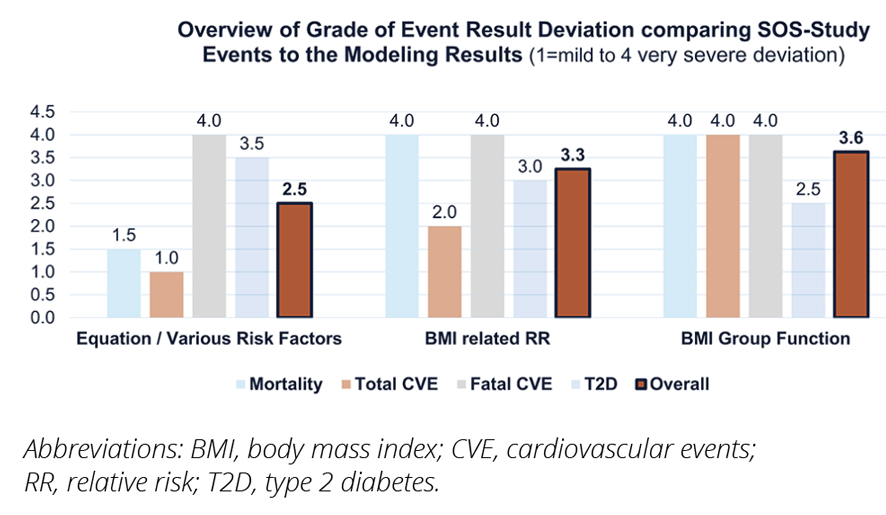
Figure 4. Comparison of Main Incremental Health Economic Outcomes
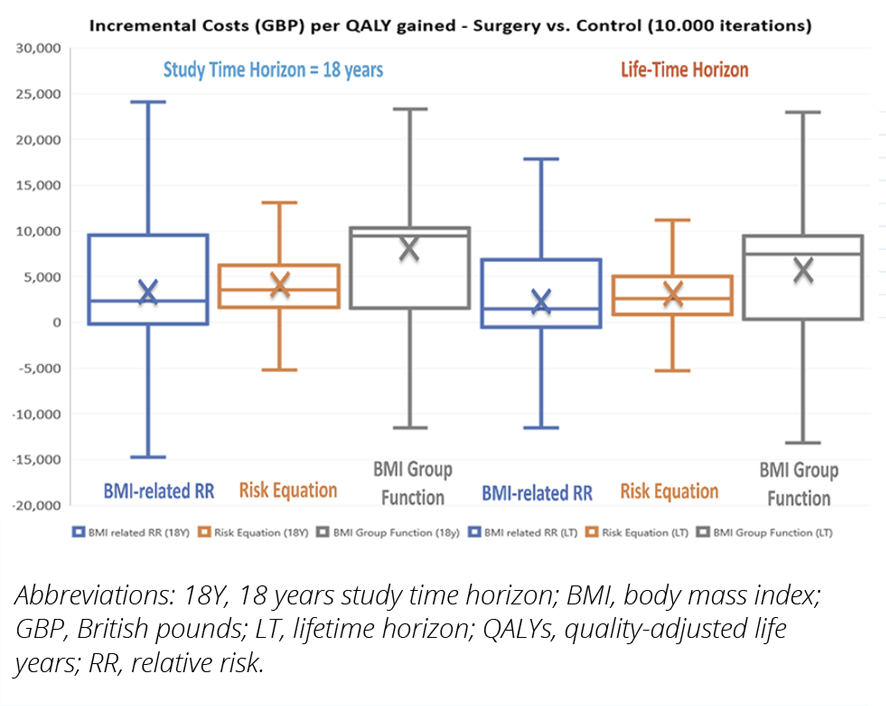
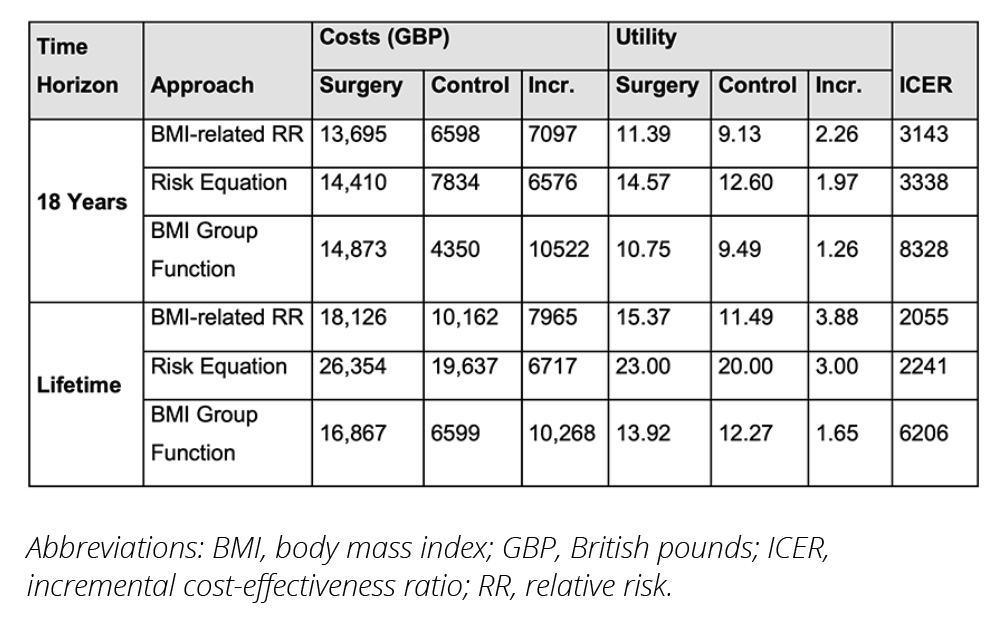
To investigate the potential impact of the different event-simulation approaches on the health economic key results, namely the incremental costs the incremental QALYs and the ICER, model simulations were performed comparing surgery versus controls. All models were informed by the same cost and health utility data, extracted from a recent UK NICE appraisal on obesity,18 as well as by the same population and effect input data from the SOS-study, to ensure comparability. Model simulations were performed for an 18-year SOS-study time horizon and for a lifetime horizon, using Monte Carlo simulations with 10,000 iterations to consider the variation of results. These results are presented in Table 1 (showing the mean cost, QALY, and ICER results), and in Figure 4 (showing the ICERs and the deviation of ICERs as boxplots). Considering the mean results presented in Table 1, the ICER was lowest for the BMI-related RR approach, followed by the risk equation approach, and was highest for the BMI group function, irrespective of the model time horizon. Looking at these mean results, the BMI-related RR approach consistently demonstrates the best cost-effectiveness, especially as it achieves higher QALYs for its cost difference, compared with the other approaches. Conversely, the BMI group function approach, having the highest costs and lowest QALYs in most cases, generally results in the least favorable ICERs.
However, looking at the distribution of the ICER values, presented in Figure 4, the different confidence interval levels presented in the box plots are largely overlapping, making the ICER outcomes comparable from a statistical point of view.
Table 1. Overview of Mean Health Economic Outcomes
Summary and Impact
The findings of our research answered 2 central questions that are strongly connected to trust and confidence in health economic models.
- How complex does a HE obesity model need to be to adequately predict obesity-associated events? This study suggests that the structure of a HE model matters if clinical events are to be predicted most accurately. Although it was found that none of the structural approaches showed perfect external event validation results, the risk equation approach showed the smallest deviations. Combined with a careful selection of risk equations, this risk equation approach would be the method of choice for a most accurate prediction of obesity-associated events.
- What impact has the modeling approach on the HE results? If the purpose of an HE model is purely the incremental HE comparison, this study suggests that the structure does not matter much, which seems positive for the credibility and comparability of HE key results based on different structural modeling approaches. The different structural approaches provided comparable probabilistic health economic results, whereas looking at the mean results (in a purely deterministic manner), the categorical BMI approach produced the highest mean ICER and is hence the most conservative estimate from a modeler’s perspective (the most cautious in estimating costs, benefits, or outcomes).
"This study suggests that the structure of an HE model matters if clinical events are to be predicted most accurately."
The findings of our research are based on the limitation of using the SOS study as basis. This bases this research on a population of patients with severe obesity (reflected by a mean BMI ≥40 mg/m² in the SOS study population). Furthermore, the surgical approach used in the SOS study is the most invasive and (in the long-term) most efficient intervention approach in obesity. This means that the observed variations in BMI and other risk factors, which are translating into disease risk changes and so into the number of events simulated, related costs, and related QALYs, are strongest for surgery compared to any other less-invasive obesity intervention. Although the surgery option is not representative, it reflects an extreme scenario, in which differences between the investigated structural event simulation approaches should be most pronounced. As in this “extreme scenario” no significant difference was observed, it is likely that these results are transferable to other obesity interventions (such as tirzepatide or semaglutide), although additional research is required to confirm this hypothesis. One key requirement to inform future research in this field are other long-term studies, best representing other obesity interventions, which would allow reperforming this research in a broader population of people with obesity.
References
- Schwander B. Systematic evaluation, replication and validation of structural health economic modelling approaches: Lessons learned in the field of obesity [doctoral thesis]. Maastricht, The Netherlands: Maastricht University; 2023.
- WHO Health Topics – Obesity. World Health Organization. https://www.who.int/health-topics/obesity. Published 2024. Accessed January 15, 2025.
- Obesity and Overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published March 1, 2024. Accessed January 15, 2025.
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403(10431):1027-1050.
- Economic impact of overweight and obesity to surpass $4 trillion by 2035. World Obesity Association. https://www.worldobesity.org/news/economic-impact-of-overweight-and-obesity-to-surpass-4-trillion-by-2035. Accessed April 21, 2024.
- Willis M, Johansen P, Nilsson A, Asseburg C. Validation of the economic and health outcomes model of type 2 diabetes mellitus (ECHO-T2DM). Pharmacoeconomics. 2017;35(3):375-396.
- Lopes S, Johansen P, Lamotte M, McEwan P, Olivieri A-V, Foos V. External validation of the core obesity model to assess the cost-effectiveness of weight management interventions. Pharmacoeconomics. 2020;38(10):1123-1133.
- D’Agostino RB, Russell MW, Huse DM, et al. Primary and subsequent coronary risk appraisal: new results from the Framingham study. Am Heart J. 2000;139(2 Pt 1):272-281.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22(3):312-318.
- Clarke PM, Gray AM, Briggs A, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia. 2004;47(10):1747-1759.
- Ara R, Blake L, Gray L, et al. What is the clinical effectiveness and cost-effectiveness of using drugs in treating obese patients in primary care? A systematic review. Health Technol Assess. 2012;16(5):iii-xiv, 1-195.
- Au N, Marsden G, Mortimer D, Lorgelly PK. The cost-effectiveness of shopping to a predetermined grocery list to reduce overweight and obesity. Nutr Diabetes. 2013;3(6):e77.
- Caro J, Stillman O, Danel A, Getsios D, McEwan P. Cost effectiveness of rimonabant use in patients at increased cardiometabolic risk: estimates from a Markov model. J Med Econ. 2007;10(3):239-254.
- Meads DM, Hulme CT, Hall P, Hill AJ. The cost-effectiveness of primary care referral to a UK commercial weight loss programme. Clin Obes. 2014;4(6):324-332.
- Schwander B, Nuijten M, Hiligsmann M, et al. Identification and expert panel rating of key structural approaches applied in health economic obesity models. Health Policy Techn. 2020;9(3):314-322.
- McManus E, Turner D, Sach T. Can you repeat that? Exploring the definition of a successful model replication in health economics. Pharmacoeconomics. 2019;37(11):1371-1381.
- Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219-234.
- Single Technology Appraisal - Liraglutide for managing overweight and obesity [ID740]. National Institute for Health and Care Excellence. https://www.nice.org.uk/guidance/ta664/evidence/appraisal-consultation-committee-papers-pdf-8952596893. Published 2020. Accessed January 19, 2022.