White Paper
The Future of HE+OR:
HEOR’s and ISPOR’s Impact on Healthcare Systems and the Multistakeholder Community
Background – Global Complexity of Healthcare
 The healthcare ecosystem is under immense pressures around the globe. While many stakeholders struggle with similar issues, they meet those issues with differing priorities depending on where in the world one lives and which perspective is used to view these major shifts that are occurring. Demographics are rapidly shifting worldwide for a variety of reasons. The good news is that many populations are experiencing improved levels of health. As life expectancies have continued to rise in general, the proportion of people aged 60 and older is set to increase 56% between 2015 and 2030.1 The trajectory of health spending in 37 of the Organization for Economic Cooperation and Development (OECD) countries is again growing, on average, after the economic slowdown in 2008.2 Healthcare spending represented, on average, approximately 9% of GDP in 2016 and was on track to remain the same in 2017 in OECD countries. However, this does mask wide variation within the countries represented, ranging from 4.2% to 17.2%. While some low- and middle-income countries (LMIC) are making good progress toward collectively funded healthcare systems (eg, China), lower-income countries continue to struggle with the ongoing challenge of providing basic healthcare.3
The healthcare ecosystem is under immense pressures around the globe. While many stakeholders struggle with similar issues, they meet those issues with differing priorities depending on where in the world one lives and which perspective is used to view these major shifts that are occurring. Demographics are rapidly shifting worldwide for a variety of reasons. The good news is that many populations are experiencing improved levels of health. As life expectancies have continued to rise in general, the proportion of people aged 60 and older is set to increase 56% between 2015 and 2030.1 The trajectory of health spending in 37 of the Organization for Economic Cooperation and Development (OECD) countries is again growing, on average, after the economic slowdown in 2008.2 Healthcare spending represented, on average, approximately 9% of GDP in 2016 and was on track to remain the same in 2017 in OECD countries. However, this does mask wide variation within the countries represented, ranging from 4.2% to 17.2%. While some low- and middle-income countries (LMIC) are making good progress toward collectively funded healthcare systems (eg, China), lower-income countries continue to struggle with the ongoing challenge of providing basic healthcare.3
The complexity of healthcare decision making continues to intensify. Innovative treatments with curative potential based on precision/personalized medicine have become a reality. However, these cutting-edge therapies complicate the value-determination process of patients, payers, and society and accordingly, the healthcare budget-planning process. The increasingly complex innovative treatment options, combined with the growing focus on healthcare equity and increased access to healthcare encouraged by the World Health Organization (WHO),4 present a challenging combination of issues for decision makers. In order to meet challenges in each country, definitions of value will need to include multiple perspectives and local contexts, while new approaches to managing affordability should be considered, too. Additionally, a strengthening of existing approaches to healthcare evaluation and the development of new approaches that balance scientific and deliberative processes may provide both further rigor and transparency in decision making.
The complexity of healthcare decision making continues to intensify.
HEOR Defined
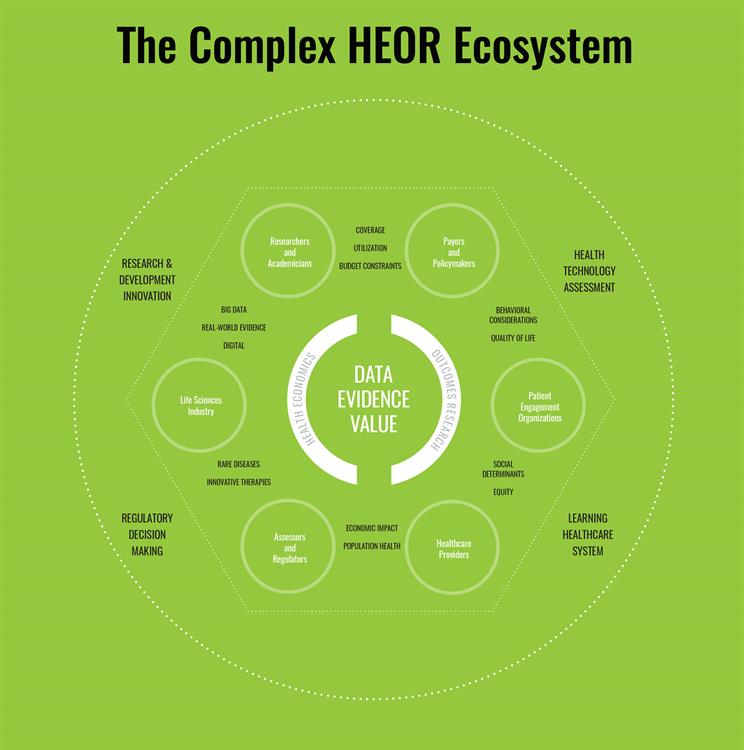
Health economics and outcomes research (HEOR) provides a framework that can clearly define healthcare issues and generate and assemble the relevant evidence to inform and guide healthcare-related decision making in this constantly evolving space. HEOR entails providing and evaluating a range of economic and outcomes data, showing how decision alternatives impact outcomes and influence stakeholders, with the intention to guide healthcare-related investment decisions; inform behaviors of key stakeholders; comparatively evaluate outcomes; and measure quality within the healthcare system. HEOR is the confluence of 2 fields that work together to provide powerful data and insights for healthcare decision makers.
In its application in HEOR, health economics has tended to focus on the measuring and valuing the outcomes of healthcare interventions. However, health economics is also concerned with wider issues relating to the behavior of healthcare markets, the performance of systems for funding, and providing healthcare, including policy-oriented issues (such as reference pricing and intellectual property incentives).
Outcomes research comprises a set of scientific disciplines—with clinical, public health, social, and humanistic elements—that evaluate the effect of healthcare interventions in terms of clinical endpoints and economic outcomes. Outcomes research is generally based on the conceptual framework that involves comparison and evaluation of treatment alternatives including the simultaneous assessment of multiple types of outcomes that are health related. The conduct of outcomes research involves not only epidemiologic and real-world data, but also patient-reported outcomes, biostatistics, clinical studies, systematic reviews, and meta-analyses. Outcomes research is a key partner to health economic analysis in that it provides the underpinnings and fuller understanding of patient outcomes that are crucial to a well-informed health economic evaluation.
HEOR is the confluence of 2 fields that work together to provide powerful data and insights for healthcare decision makers.
The Role of HEOR in Improving Healthcare Decision Making
Multidisciplinary experts in HEOR understand that outcomes research combined with health economics provides vital information and tools to healthcare decision makers from the intervention to the healthcare system level. While both health economics and outcomes research can be performed in isolation, the synergy of combining the right data (outcomes research) with thoughtful (health) economic analyses based on multiple stakeholder perspectives ensures that even complex healthcare questions can be evaluated rationally. This is the unique strength of HEOR in the healthcare space. While some experts focus in one space or the other, HEOR experts can dive deep in their area of expertise but also understand the value of incorporating the views and outputs from complementary disciplines, striving to build bridges between data and economic analysis, often starting the data plan with the end in mind so that all the relevant outcomes can be applied or collected from varying sources of data and analyzed from varying perspectives.
Health technology assessors particularly understand this approach. They appreciate that using credible data from all areas of a healthcare system and over the entire lifecycle of a health technology (even when extrapolated) is often the only way to assess long-term costs and benefits. This approach provides an evidence base by which to determine the most cost-effective choice within budget-constrained environments like healthcare. For example, the recommendation to provide human papilloma virus vaccination for both boys and girls by Ireland’s Health Information and Quality Authority (HIQA) was based on cost-effectiveness analyses.5 Other examples of agencies that rely on health technology assessment (HTA) include the National Institute for Health and Care Excellence (NICE) in the United Kingdom, the Institute for Clinical and Economic Review (ICER) in the United States, and the Health Insurance Review and Assessment Service (HIRA) in South Korea.
Single (government) payers have been using HTA2 for decades. Value-based healthcare evaluation (including value-based insurance design and pricing), learning healthcare systems, and an increased emphasis on placing patients at the center of healthcare decisions are putting more focus on the confluence of HEOR as a key evidence-generating aspect for assessment. Paying for value requires first defining what value is and to whom that value matters (what perspective), measuring the care delivered in real time, and feeding that information back into the system so adjustments can be made to incentivize and reimburse high-value care appropriately. Methods developed over the past 3 decades compare the clinical, economic, and humanistic impact of alternative treatments and provide the basis for addressing evolving challenges, including personalized medicine, curative therapies, and aging populations. New methods will need to take a holistic view in terms of time horizon, societal benefit, opportunity cost, and affordability. HEOR experts and methods are often the vanguard of healthcare evaluations with dynamic, innovative methods to address the constantly changing environment.
While both health economics and outcomes research can be performed in isolation, the synergy of combining the right data (outcomes research) with thoughtful (health) economic analyses based on multiple stakeholder perspectives ensures that even complex healthcare questions can be evaluated rationally.
The Future of HEOR
The rise of “big data” and a focus on artificial intelligence mean that healthcare data are becoming more abundant and diverse, useful, and able to impact healthcare decisions in real time. The promise and power of healthcare data can be realized with real-time insights to drive change in treatment, measure quality, and enable (cost-) efficient healthcare delivery. However, much of the data content is in unstructured form (eg, physician notes in electronic medical records), and natural language processing has not been very effective in extracting content. Expertise in deep-learning methods as well as knowledge of traditional outcomes research methods and good practices will be key to delivering on the promise of big data.
Genetic data, including data from companion diagnostics, and the need for interoperability to link disparate data sets together will exponentially increase the size of data sets and their usability to detect and analyze trends. This will expand the breadth of HEOR skill sets to analyze and communicate what this means for patients, payers, and healthcare systems. The proliferating digitization of healthcare data and development of algorithms that can rapidly discover (virtually at the time of collection) actionable trends, while measuring outcomes in meaningful ways, will increase the applicability and impact of HEOR methods. This significant trend will allow learning healthcare systems to come to the forefront. Both Kaiser Permanente and Geisinger Health Systems in the United States are active examples of integrated delivery network research influencing practice and in turn, practice influencing research.
HEOR can also help ensure more systematic yet customizable approaches to healthcare evaluation in different parts of the world. There is massive variation in decision-making capacity across regions highlighted by the backdrop of fiscal challenges in the LMIC. The regions often most in need of decision-making tools have limited resources or capacity to develop and execute these types of analyses. These regions require revision of the mindset when developing optics, methods, and communications strategies regarding evidence-based decision making, for example, by applying the transparency, accountability, participation, integrity, capacity (TAPIC) framework.4
Expertise in deep-learning methods as well as knowledge of traditional outcomes research methods and good practices will be key to delivering on the promise of big data.
HEOR Stakeholders
HEOR is performed and/or used by many different types of decision makers. Some are experts at the forefront of developing new methods to inform evidenced-based decision making. However, decision makers are often in other related disciplines who may not recognize that the work they are doing is HEOR. Traditionally, HEOR experts work in the health technology sector (eg, biopharma, traditional pharmaceutical, medical device and diagnostics, and health informatics industries); in HTA; and in academic centers that focus on health economics, epidemiology, systematic evidence reviews, or related research methods. However, other consumers of HEOR data/tools such as regulators, patients, providers (eg, health systems, practices, physicians), payer/budget holders, actuaries, and health IT professionals (including data scientists) are all struggling with healthcare decisions that often involve HEOR questions. Patients and caregivers are one of the highest priority groups because much of the data that go into outcomes research and health economic analyses start at the patient level. Importantly, patients and caregivers are the ultimate beneficiaries of any healthcare decision based on that evidence. Obtaining feedback, buy-in, and participation by patients or their representatives is imperative to the evidence-based process of defining and determining value at the core of HEOR. Understanding and measuring outcomes that patients and society value is key to ensuring that healthcare resources yield the most benefit possible. This includes a clear understanding of the (health) benefits that are likely to be displaced as a consequence of a decision to invest in a new technology. Healthcare systems and providers need outcomes and cost data to inform real-time, evidence-based decisions at both the system and the patient levels, including understanding how performance compares to other benchmarks for quality feedback. These data can also inform patient-level decisions (eg, providing the right patient, the right drug, the right dose, at the right time and in the right location) and eventually discussions about out-of-pocket costs prior to prescribing.
Regulatory and HTA bodies are large consumers of data, particularly for new pharmaceuticals. The “base data set” for assessments of this kind is traditional clinical studies: randomized controlled trials (RCTs)—where HEOR researchers work closely with clinical study teams to include HEOR endpoints and other data collection needed to provide the broader perspective. Increasing collaboration between clinical research and HEOR offers opportunities to make traditional RCTs more relevant to real-world clinical practice and create complementary HEOR studies and tools that are tailored to the full set of questions the healthcare system needs to answer in order to provide high-value care efficiently. The confluence of these data coming from the outcomes research space enables understanding of how performance of technology differs between real-world settings and more controlled clinical trial settings.
In day-to-day healthcare practice, healthcare technologies are often used in populations and under conditions that are not part of controlled research settings. These circumstances can impact the magnitude of benefit, the volume of patients treated, and subsequently the cost of care. HEOR analyses often include these uncertainties as part of their analysis of the healthcare situation. This is becoming a vital part of technology uptake in healthcare and has long been used by HTA agencies to provide the evidence that payers/budget holders use in the coverage determination process. Increasingly, this is requiring adaptive processes that permit conditional reimbursement to provide early access to those most in need, collecting data to further assess safety and effectiveness, and reassessing the technology based on these real-world data. Other data scientists are often collaborators with HEOR experts, and many of the methods cross over with actuarial science, biostatistics, psychology, and economic methods. Many of the good practices in these and other areas of data analytics are informed by good practices that were developed in the field of HEOR.
Clearly, the scientific and clinical ecosystem surrounding HEOR is complicated. HEOR experts take outcomes data and defined value parameters and apply the lens of the current external perspectives and healthcare challenges (often in partnership with those affected or needing the information) to produce useful tools and evidence that can be used by the various collaborators or end users.
HEOR is performed and/or used by many different types of decision makers.
ISPOR and HEOR
ISPOR, the leading professional society for HEOR globally, was established in 1995 by a small group of dedicated volunteers and visionaries with the goal of advancing the science and practice of HEOR around the world. As the field of HEOR has grown globally, so has ISPOR. The Society's membership has expanded from just 240 members at its founding to more than 20,000 individual and chapter members from 110+ countries worldwide. As a multidisciplinary organization, the Society's membership includes a wide variety of healthcare stakeholders, including researchers and academics, assessors and regulators, payers and policy makers, the life sciences industry, healthcare providers, and patient engagement organizations.
ISPOR’s mission is to promote health economics and outcomes research excellence to improve decision making for health globally. The Society’s strategic goals include scientific and research excellence, communication and collaboration, education and training, and member or stakeholder engagement. ISPOR is committed to strengthening the integrity and advancing the understanding and use of HEOR research. This extends to being known as a reliable and valued resource for translating knowledge into practice, and building knowledge and skills including leading efforts to strengthen and expand capabilities in HEOR for all our members and other stakeholders, including providers, HTA bodies, payers, patients, health authorities, and other professional societies.
ISPOR’s mission is to promote health economics and outcomes research excellence to improve decision making for health globally.
Authors
Federico Augustovski, MD, MSc, PhD, Institute for Clinical Effectiveness and Health Policy; Finn Børlum Kristensen, MD, PhD, University of Southern Denmark; William H. Crown, PhD, OptumLabs; Nancy J. Devlin, PhD, University of Melbourne; Nancy S. Berg, ISPOR; Ramiro Gilardino, MD, MSc, ISPOR; Lucinda Orsini, DPM, MPH, ISPOR; and Richard J. Willke, PhD, ISPOR
References
- Hasseltine WA. Aging populations will challenge healthcare systems all over the world. Forbes. https://www.forbes.com/sites/williamhaseltine/2018/04/02/aging-populations-will-challenge-healthcare-systems-all-over-the-world/#7c6fc9aa2cc3. Published April 2, 2018. Accessed December 5, 2018.
- Focus On: Spending on Health: Latest Trends OECD 2018 June www.oecd.org/health. Published June 2018. Accessed September 29, 2019.
- New Perspectives on Global Health Spending for Universal Health Coverage. Geneva, Switzerland: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
- Tracking Universal Health Coverage: 2017 Global Monitoring Report. World Health Organization and International Bank for Reconstruction and Development / The World Bank; 2017. Licence: CC BY-NC-SA 3.0 IGO.
- Health technology assessment (HTA) of extending the national immunization schedule to include HPV vaccination of boys. Health Information and Quality Authority. https://www.hiqa.ie/sites/default/files/2018-12/HTA-for-HPV-Vaccination-boys.pdf. Published December 4, 2018. Accessed January 30, 2019.
